ACLS Acute Coronary Syndrome (ACS) Algorithm
The most frequent symptom of Acute Coronary Syndrome (ACS) is chest pain, which often leads patients to the emergency medical department. The ACLS Acute Coronary Syndrome (ACS) algorithm is designed to help healthcare providers quickly assess and manage these situations. ACS can be triggered by a range of factors, from harmless to life-threatening. In addition to chest pain, symptoms may include chest discomfort, shortness of breath, nausea, lightheadedness, and sweating. Proper evaluation and prompt treatment using the ACS algorithm are essential to minimize heart damage and prevent complications.
The three conditions of acute coronary syndrome (ACS) are:
- Non-ST-segment Elevation Myocardial Infarction (NSTEMI)
- ST-segment Elevation Myocardial Infarction (STEMI)
- Unstable Angina
The goal of the emergency department is to determine the cause of the discomfort and initiate appropriate medication.
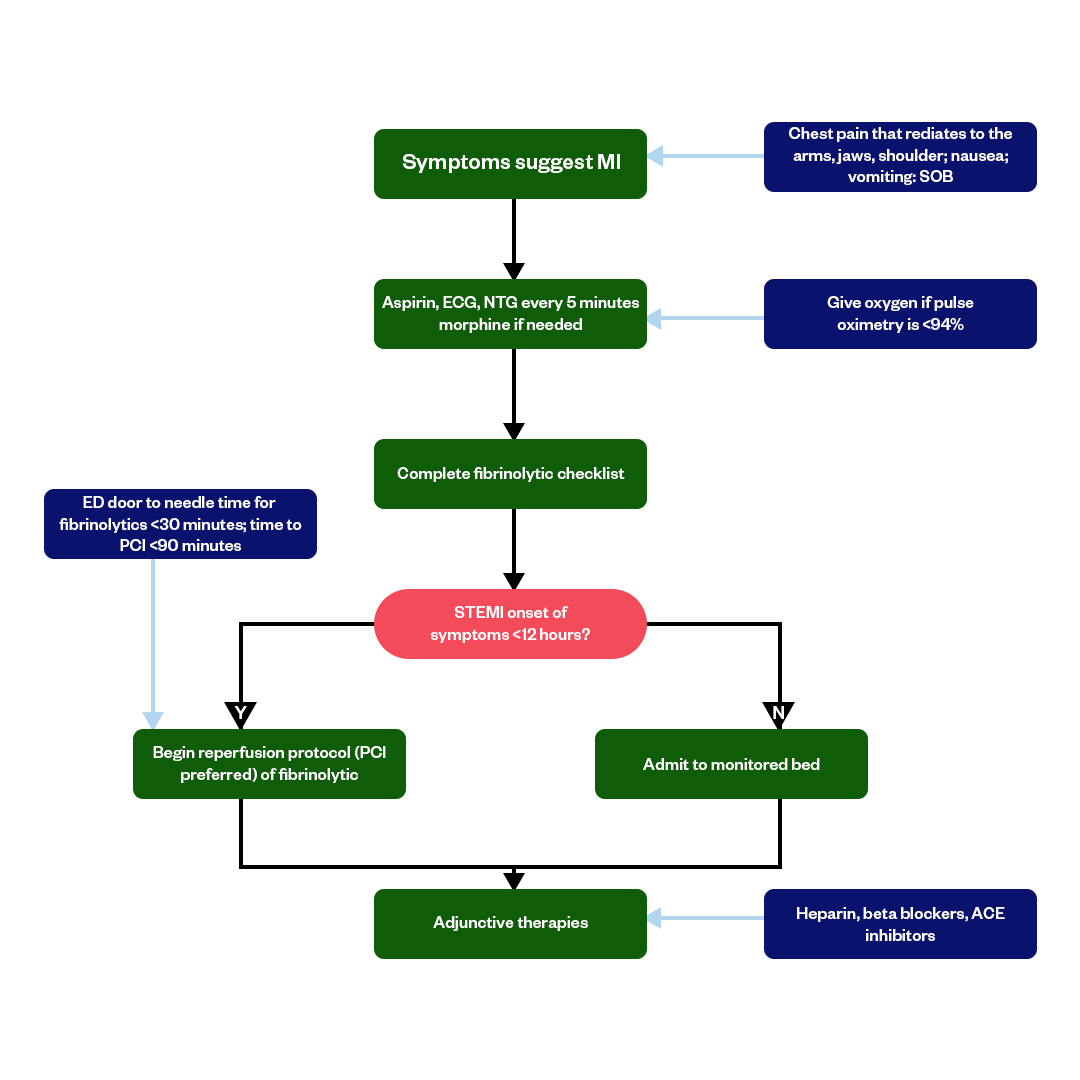
Acute Coronary Syndrome (ACS) Treatment Algorithm
Before any treatment begins, early identification of Acute Coronary Syndrome (ACS) is essential. According to American Heart Association guidelines, prompt recognition of conditions such as ST elevation myocardial infarction (STEMI), ventricular tachycardia, and potential cardiac arrest is critical. Immediate response improves life support efforts and leads to better overall patient care outcomes. It’s also crucial to note that the management of ACS should be individualized based on the patient's specific clinical presentation, underlying risk factors, and the resources available at the point of care.
Here are the key steps you should follow in the ACS treatment algorithm:
1. Initial Assessment and Recognition:
- Promptly recognize and assess patients presenting with symptoms suggestive of ACS, such as chest pain or discomfort.
- Perform an initial evaluation, including a medical history, physical examination, and an electrocardiogram (ECG) to identify changes indicative of ACS.
2. Immediate Treatment:
- Administer oxygen if the patient is hypoxic.
- Provide aspirin (chewed or crushed) to all patients without contraindications, which helps inhibit platelet aggregation.
- Administer nitroglycerin sublingually or through an intravenous route to relieve chest pain or discomfort if blood pressure is not too low.
3. Establishing a Diagnosis:
- Continue with diagnostic tests, including serial ECGs, cardiac biomarker (troponin) measurements, and additional imaging (e.g., echocardiography or stress testing) as necessary.
- ST-segment elevation on the ECG often indicates ST-elevation myocardial infarction (STEMI). In contrast, non-ST-segment elevation ACS (NSTE-ACS) includes non-ST-segment elevation myocardial infarction (NSTEMI) and unstable angina.
4. Risk Stratification:
- Assess the patient's risk factors, clinical presentation, and ECG findings to stratify the risk of adverse outcomes.
- Identify high-risk features, such as hemodynamic instability, arrhythmias, or ongoing chest pain, which may require more aggressive interventions.
5. Revascularization:
- For STEMI patients, primary percutaneous coronary intervention (PCI) is the preferred reperfusion strategy if available within a reasonable time frame.
- For NSTE-ACS patients, deciding to proceed with early invasive strategies (PCI or coronary artery bypass grafting) depends on the risk assessment and clinical stability.
6. Medical Therapy:
- Administer medications, including antiplatelet agents (clopidogrel, prasugrel, ticagrelor), anticoagulants, beta-blockers, angiotensin-converting enzyme (ACE) inhibitors, and statins, as appropriate, based on the patient's condition and comorbidities.
7. Ongoing Monitoring:
- Continuously monitor the patient's vital signs, ECG, and symptoms.
Adjust treatment and interventions based on the patient's response and evolving clinical status.
8. Secondary Prevention:
- Provide counseling and education on lifestyle modifications, medication adherence, and risk factor management.
- Develop a plan for long-term secondary prevention, including medications and cardiac rehabilitation.
Fast and Convenient
Take ACLS Classes
*Nationally Accepted
ACLS
CERTIFICATION
AHA ACLS course
State-of-the-Art Facilities
Unlimited Exam Retakes
$260
ACLS
ONLINE CERTIFICATION
AHA ACLS Online Course
100% online training
Unlimited Exam Retakes
$280
Acute Coronary Syndrome FAQs
What is an acute coronary syndrome algorithm?
Acute coronary syndrome is a term to describe the condition of reduced blood flow to the heart. An acute coronary syndrome algorithm is a step-by-step medical decision-making tool healthcare professionals use to intervene in cardio-related emergencies.
What is the first 10 minutes of ACLS ACS?
Assessment and stabilization of the patient should occur within the first 10 minutes of ACS. In the first 10 minutes of ACLS for ACS, assess ABCs (Airway, Breathing, and Circulation), attach monitoring equipment, Give oxygen, perform a 12-lead ECG, manage pain, and administer aspirin.
What are the three conditions of ACS?
Non-ST-segment elevation myocardial infarction (NSTEMI), ST-segment elevation myocardial infarction (STEMI), and unstable angina are the three conditions of Acute Coronary Syndrome (ACS). STEMI is considered more severe than NSTEMI due to the complete blockage of a coronary artery. Although both are types of heart attacks and need urgent care, following the ACLS protocol helps healthcare providers respond quickly and treat each condition.
What is the most common cause of acute coronary syndrome ACS?
ACS is caused due to plaque disruption in the coronary arteries of the heart (atherosclerosis). The most common risk factors for the disease are atherosclerosis, coronary artery spasm, dissection, embolism, drug use, certain medications, heredity, diabetes, obesity, and high cholesterol.
What is the primary goal of the ACS algorithm?
The primary goal of the ACS algorithm is to figure out the cause of ACS or heart attack and stabilize the patients. The algorithm includes initial assessment and recognition, diagnosis and medication, medical therapy, and ongoing monitoring. Learn more in detail in this article.

Owner Jeff Haughy has been providing high-quality care in the EMS industry since 1995 and started his Fire Service career with the Alameda Fire Department in 1991 as a Fire Explorer.