Pediatric BLS Algorithm
Scope of Guidelines
The scope of guidelines for pediatric Basic Life Support (BLS) algorithms is intended to be a systematic approach to providing life-saving interventions for infants and children in cardiac arrest or situations of compromised cardiopulmonary function. The BLS algorithm guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care (CPR-ECC) are reviewed by the International Liaison Committee on Resuscitation (ILCOR) under the evidence of clinical and laboratory results. The guidelines are published jointly by ILCOR, the American Heart Association (AHA), and the European Resuscitation Council (ERC).
The pediatric BLS algorithm guidelines outline the sequence of actions required to optimize outcomes. The algorithm covers critical aspects such as the recognition of:
- Cardiac arrest
- Activation of emergency response
- Assessment of the child's
- condition
- Effective chest compressions
- Proper airway management
- Use of automated external defibrillators when appropriate
Pediatric BLS guidelines are essential for healthcare providers and lay rescuers, emphasizing the importance of early recognition and timely intervention to improve survival rates in pediatric emergencies.
The Pediatric Chain of Survival
The Pediatric Chain of Survival is a vital concept in pediatric emergency medicine, delineating a series of critical steps aimed at optimizing outcomes for children facing life-threatening situations.
Comprising four interconnected links, it begins with prevention, emphasizing the importance of injury and illness prevention strategies.
The second link underscores the need for early recognition and activation of the emergency response system upon identifying a critical event.
The third link emphasizes high-quality pediatric BLS and advanced life support, including effective CPR and appropriate interventions.
The final link highlights the significance of post-cardiac arrest care, ensuring seamless transition and ongoing management for improved pediatric survival rates. These chain of survival is crucial for healthcare providers and first responders dedicated to pediatric emergency care.
Sequence of Resuscitation
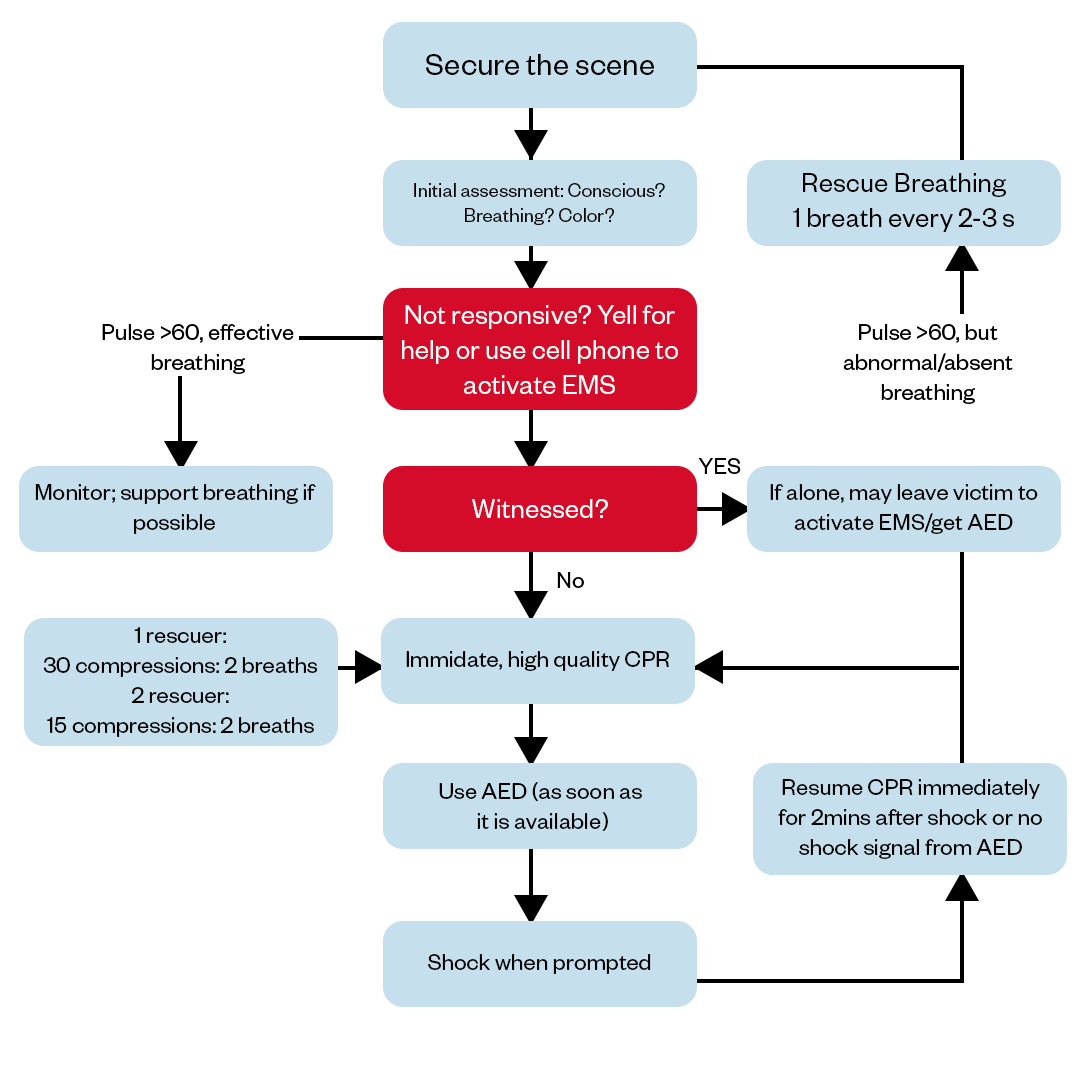
The sequence of resuscitation for pediatric patients commences with the assessment of the child's responsiveness and breathing. If the child is unresponsive or experiencing inadequate breathing, immediate activation of the emergency response system is paramount.
The next step involves the initiation of high-quality pediatric Basic Life Support (BLS), which includes chest compressions and ventilation to maintain oxygenation and circulation. Automated external defibrillators (AEDs) should be used if indicated. Once a healthcare provider arrives, advanced life support measures are implemented as needed.
Pediatric CPR
While assessing a child experiencing a cardiac medical emergency delivering high-quality chest compression, and effective ventilations are critical to improve the outcomes. Find our article on “How to perform CPR” for detailed and effective CPR delivery on different demographic victims.
The components of high-quality CPR are:
Positioning: Place the infant on a firm, flat surface, such as a backboard or a hard floor. Ensure the airway is clear of any obstructions.
Assessment: Confirm unresponsiveness and check for normal breathing. If the infant is unresponsive and not breathing normally or gasping, proceed to CPR.
Compression Technique: For infants below 1 year of age, use two fingers (index and middle) to deliver chest compressions. Place them in the center of the infant's chest, just below the nipple line.
Depth: Compress the chest to a depth of approximately 1.5 inches (4 cm). Ensure that you allow for complete chest recoil between compressions to facilitate effective blood flow.
Rate: Maintain a compression rate of 100-120 compressions per minute. This ensures adequate circulation to vital organs.
Compression-Ventilation Ratio: In infant CPR, the compression-ventilation ratio is 30:2. Administer 30 chest compressions followed by two rescue breaths.
Ventilation Technique: To provide rescue breaths, cover the infant's mouth and nose with your mouth, creating a tight seal. Deliver breaths gently to avoid excessive inflation of the lungs.
Compression and Ventilation Coordination: Coordinate compressions and ventilations effectively, minimizing interruptions to maintain consistent circulation and oxygenation.
AED Use: If an automated external defibrillator (AED) is available and the infant is unresponsive with no signs of circulation, follow the AED prompts. Attach the AED pads as directed and follow its instructions.
Continuous Assessment: Continuously assess the infant's response and monitor vital signs if additional medical assistance arrives.
Airway Interventions During CPR
During CPR, maintaining a clear and patent airway is crucial for oxygenation and ventilation. To ensure effective airway interventions, the rescuer should perform head-tilt and chin-lift or jaw-thrust maneuvers based on the child's age and suspected cervical spine injury. These maneuvers help open the airway. In infants, gentle head positioning without neck extension is essential. Additionally, the use of adjuncts like oral airways or supraglottic devices may be necessary for advanced airway management, ensuring uninterrupted oxygen supply during pediatric resuscitation efforts.
Defibrillation
Defibrillation in pediatric resuscitation is a critical intervention reserved for specific situations involving life-threatening cardiac arrhythmias, particularly ventricular fibrillation and pulseless ventricular tachycardia. Here are key points to consider:
Energy Settings: Pediatric-specific defibrillator pads or attenuators are used to reduce energy levels for infants and children. The initial dose typically ranges from 2 to 4 joules per kilogram (J/kg).
Pad Placement: Proper pad placement is essential. The anterior-posterior (AP) pad placement is standard for infants, with one pad on the front of the chest and the other on the back, while older children usually receive pads in the anterior-posterior or anterior-lateral position.
Clearance: Ensure that all individuals are clear of the patient before delivering a shock to prevent inadvertent injury.
Continuous CPR: Minimize interruptions in chest compressions. It is essential to resume CPR immediately after a shock is delivered, adhering to the recommended compression-ventilation ratio.
1 Rescuer vs. 2 Rescuer Pediatric BLS Algorithm
The main difference between 1 rescuer and 2 rescuer pediatric basic life support (BLS) is that with 2 rescuers, responsibilities can be divided so that one person focuses solely on high quality chest compressions while the other manages the airway, rescue breathing, and operation of an automated external defibrillator (AED) if available. This division of tasks allows for better coordination of care. Additionally, 2 rescuer BLS allows providers to switch compressors every 2 minutes to prevent rescuer fatigue. Overall, 2 rescuer BLS is more efficient as it distributes the physical and mental workload across multiple trained providers.
1 Rescuer Pediatric
- Assess the scene.
- Check responsiveness.
- Activate emergency response (call for help and, if available, retrieve an AED).
- Check pulse for no more than 10 seconds.
- If there is no pulse, start CPR with chest compressions at a rate of 100-120 per minute.
- After 30 compressions, give 2 rescue breaths.
- Continue the cycle of 30 compressions followed by 2 breaths until help arrives or the child starts breathing on their own.
2 Rescuer Pediatric
- Rescuer 1: Chest compressions.
- Rescuer 2: Airway and breathing (including giving rescue breaths).
- Switch roles approximately every 2 minutes (or sooner if fatigued).
- If an AED is available, Rescuer 2 should use it while Rescuer 1 continues chest compressions.
- Communicate effectively and coordinate actions to maintain an efficient CPR rhythm.
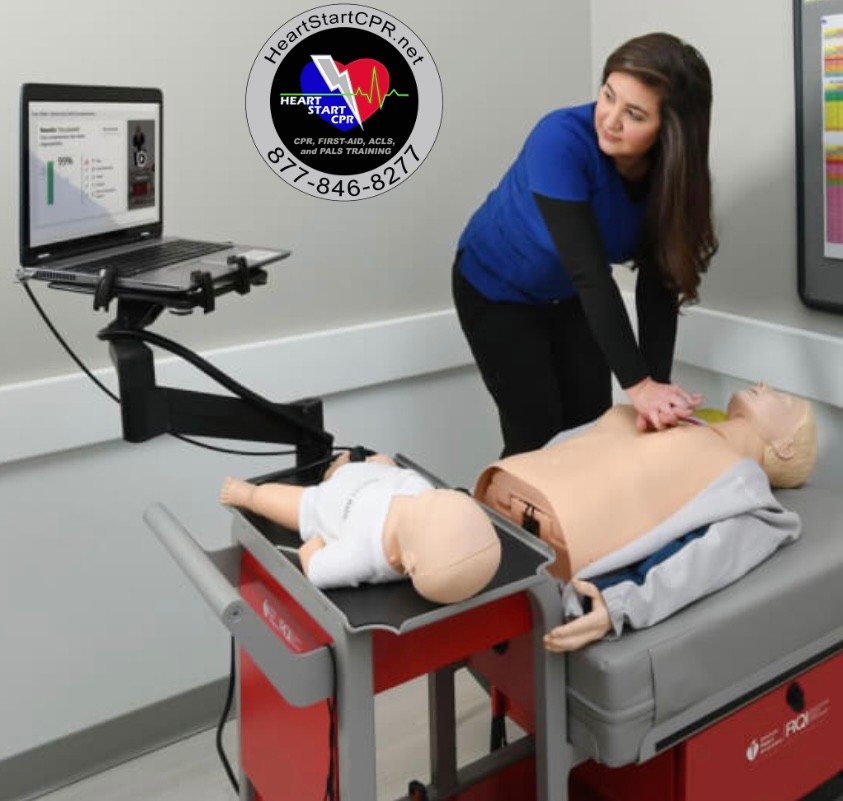
Fast and Convenient
Take BLS Classes
*Nationally Accepted
BLS
CERTIFICATION
AHA BLS course
State-of-the-Art Facilities
Unlimited Exam Retakes
$70
BLS
ONLINE CERTIFICATION
AHA BLS Online Course
100% online training
+Skills Session
$105
Pediatric BLS Algorithm FAQs
What is the sequence for BLS in a child?
It's a standard procedure to start with analyzing the environment/surrounding situations. If it's safe, then you can proceed further to follow the pediatric basic life support algorithm steps. A rescuer should act accordingly, depending on the situation. If you're a lone rescuer, then start by delivering a high-quality child CPR cycle (30 chest compressions and 2 gentle rescue breaths), assuming the child is unresponsive and has a pulse or low pulse rate. While you are on to CPR advise bystanders to seek professional medical help (Call 911 or EMS).
In the presence of multiple rescuers, one should engage in delivering 15 chest compressions while the other rescuer processes airway management. Switch roles approximately every 2 minutes (or sooner if fatigued) to prevent rescuer fatigue. Do not pause compressions for more than 10 seconds during the switch before the new compressor resumes high-quality chest compressions on the child victim. Coordinate actions efficiently between rescuers to minimize interruptions in compressions during the transition.
What pulse should a pediatric check for BLS?
The best practice is to simultaneously check breathing and pulse for no more than 10 seconds during pediatric BLS. Research shows lay rescuers are often unable to reliably detect a pulse, while stopping compressions delays vital blood flow. Therefore, the 2020 AHA Guidelines state it is reasonable for rescuers to provide CPR based on an assessment of breathing status alone.
However, healthcare providers may take the time to check for brachial ( Pulse found in the brachial artery, which runs down the upper arm in the area between the shoulder and elbow.) or femoral pulses (Pulse in the femoral artery, which runs through the thigh and groin area.) if comfortable, as pulse detection remains in the guidelines as an option to confirm the need for CPR.
Is ABC or CAB CPR for children?
Pediatric CRP follows CAB method rather than ABC, where compression comes first, followed by airway management and breaths in accordance with the newest guidelines from the American Heart Association.

Owner Jeff Haughy has been providing high-quality care in the EMS industry since 1995 and started his Fire Service career with the Alameda Fire Department in 1991 as a Fire Explorer.