PALS Algorithm
The PALS (Pediatric Advanced Life Support) algorithm is a set of guidelines and procedures designed for healthcare providers to manage pediatric emergencies.
- Shock
- Cardiac arrest
- Respiratory emergencies
- Other life-threatening emergencies
PALS algorithms focus on the advanced assessment and treatment of critically ill or injured children. The PALS guidelines are updated regularly every 5 years by the American Heart Association and American Academy of Pediatrics based upon the International Liaison Committee on Resuscitation (ILCOR) consensus on science.
The listed below algorithms are the pediatric resuscitation algorithms required in different situations of cardiac arrest. These algorithms are step-by-step assessment processes for a child patient. The Pediatric Advanced Life Support Algorithms below are helpful in hospital settings and out of the hospital setting and in passing the PALS certification/recertification exam.
Pediatric Advanced Life Support
Pediatric Cardiac Arrest Algorithm
Pediatric cardiac arrest is the cessation of cardiac mechanical activity, determined by the absence of signs of circulation. Pediatric cardiac arrest requires immediate high-quality CPR with minimal interruptions, along with early defibrillation and epinephrine administration. Key components monitored during resuscitation include chest compression fraction to ensure compressions at least 60% of the time, compression rate of 100-120 per minute, compression depth of at least one-third of anterior-posterior diameter of chest, and allowing full chest recoil after each compression. Ventilations are provided every 30 compressions for a single rescuer and 15 for two rescuers. Return of spontaneous circulation is evaluated every 2 minutes. ETCO2 and SpO2 are monitored to gauge perfusion and CPR quality
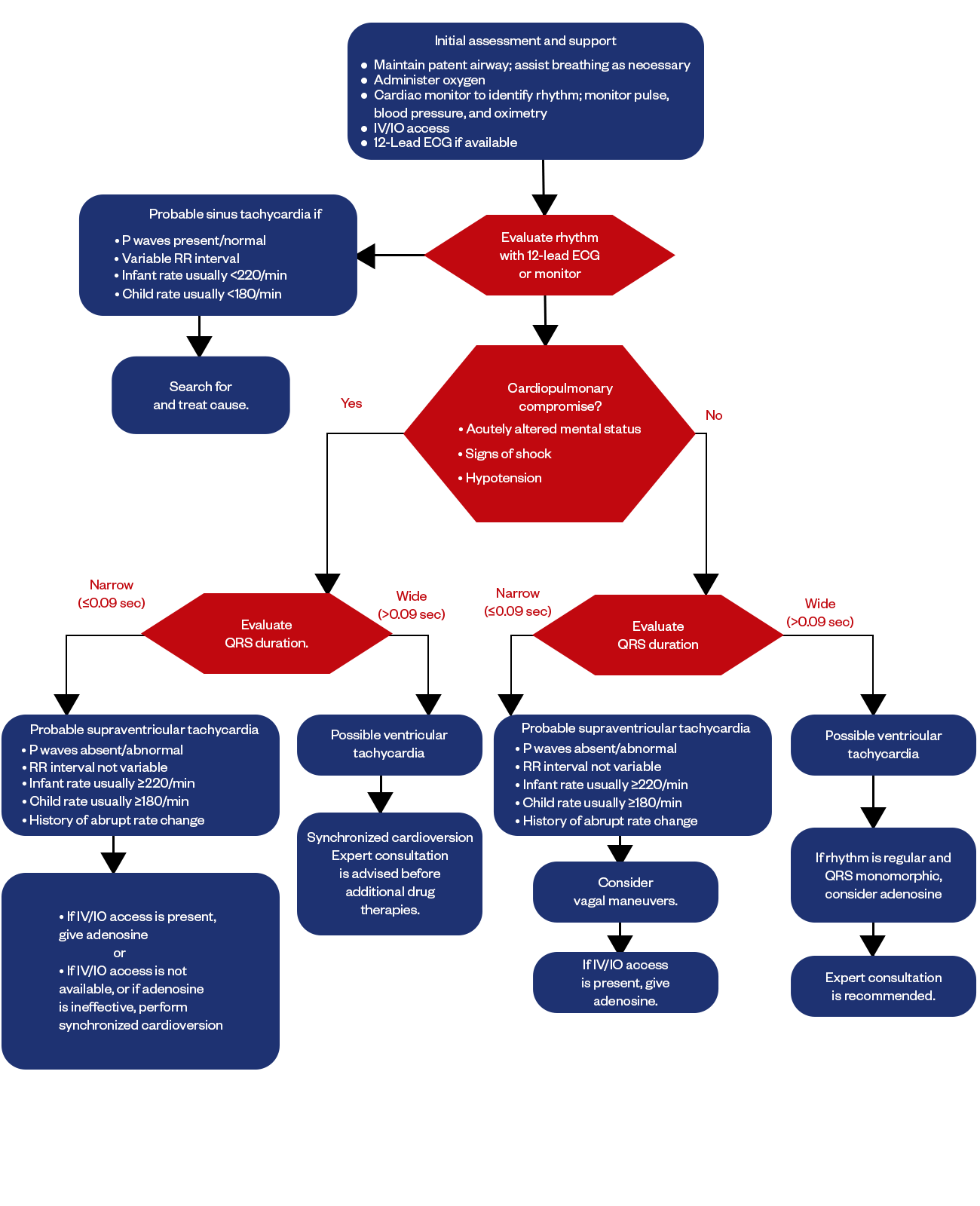
Pediatric Tachycardia With Pulse
Pediatric tachycardia refers to an abnormally fast heart rhythm in children, specifically a resting heart rate exceeding the normal limit for age. Tachycardia with pulse indicates there is maintenance of adequate cardiac output despite the fast heart rate. The approach to pediatric tachycardia involves assessment of stability, history, medications, potential causes, and the QRS duration on EKG. Stable, narrow, complex tachycardia generally suggests supraventricular tachycardia. Unstable or wide complex tachycardia suggests ventricular tachycardia. First-line treatment of stable SVT involves vagal manoeuvres like ice water to the face. Unstable SVT warrants immediate synchronized cardioversion. SVT refractory to vagal maneuvers may require adenosine or amiodarone. VT often requires cardioversion, defibrillation if pulseless, along with antiarrhythmics like amiodarone.
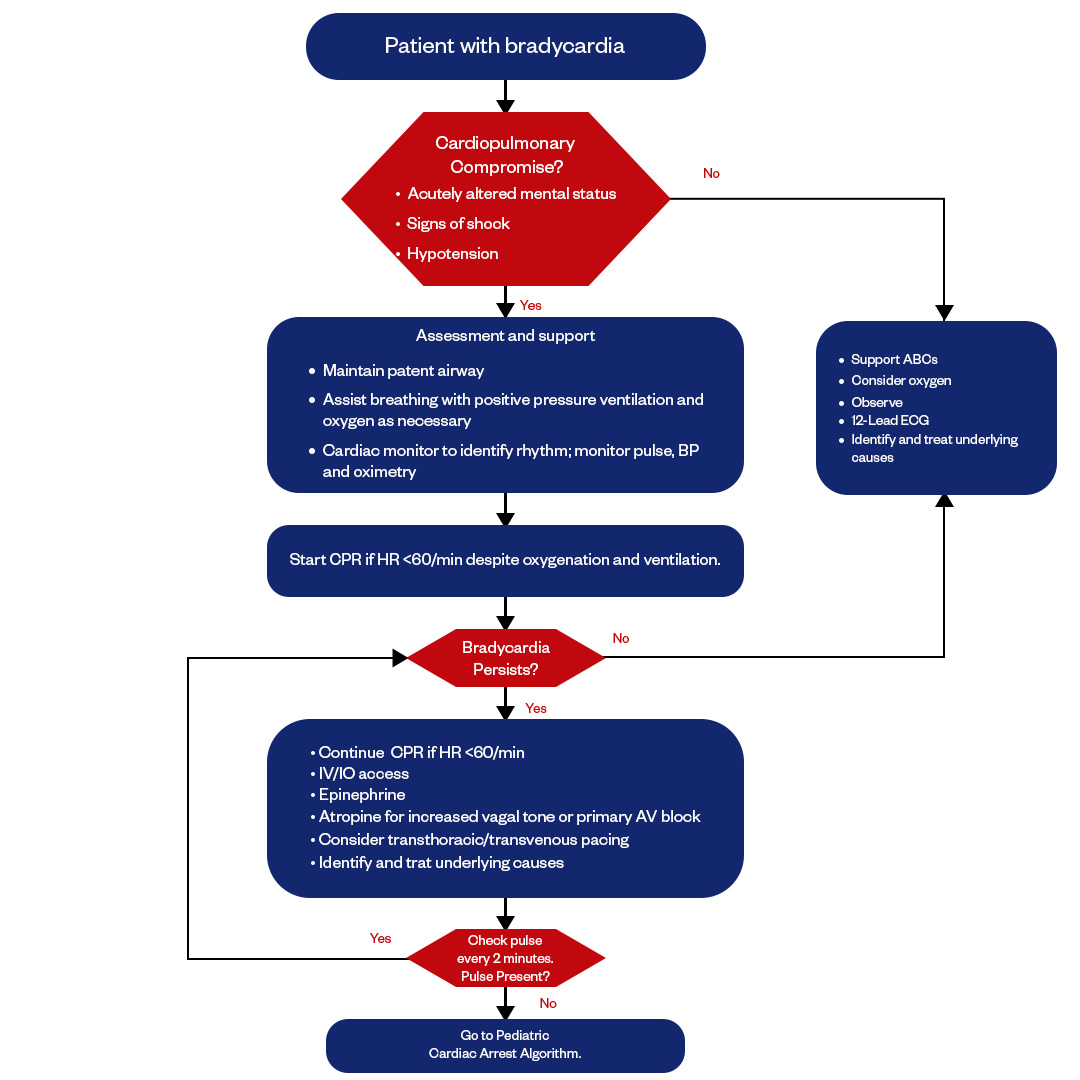
Pediatric Bradycardia With Pulse
Pediatric bradycardia refers to an abnormally slow heart rate in children, specifically a resting heart rate below the normal limits for age. Bradycardia with pulse indicates there is maintenance of adequate cardiac output and perfusion despite the slow rate. The Pediatric Bradycardia algorithm involves the assessment of signs and symptoms, identifying causes, and appropriate treatment. Symptomatic bradycardia with hypotension, altered mental status, chest pain, or heart failure warrants emergent intervention. The ultimate goal is to address the specific cause while urgently managing serious signs and symptoms related to the slow heart rate.
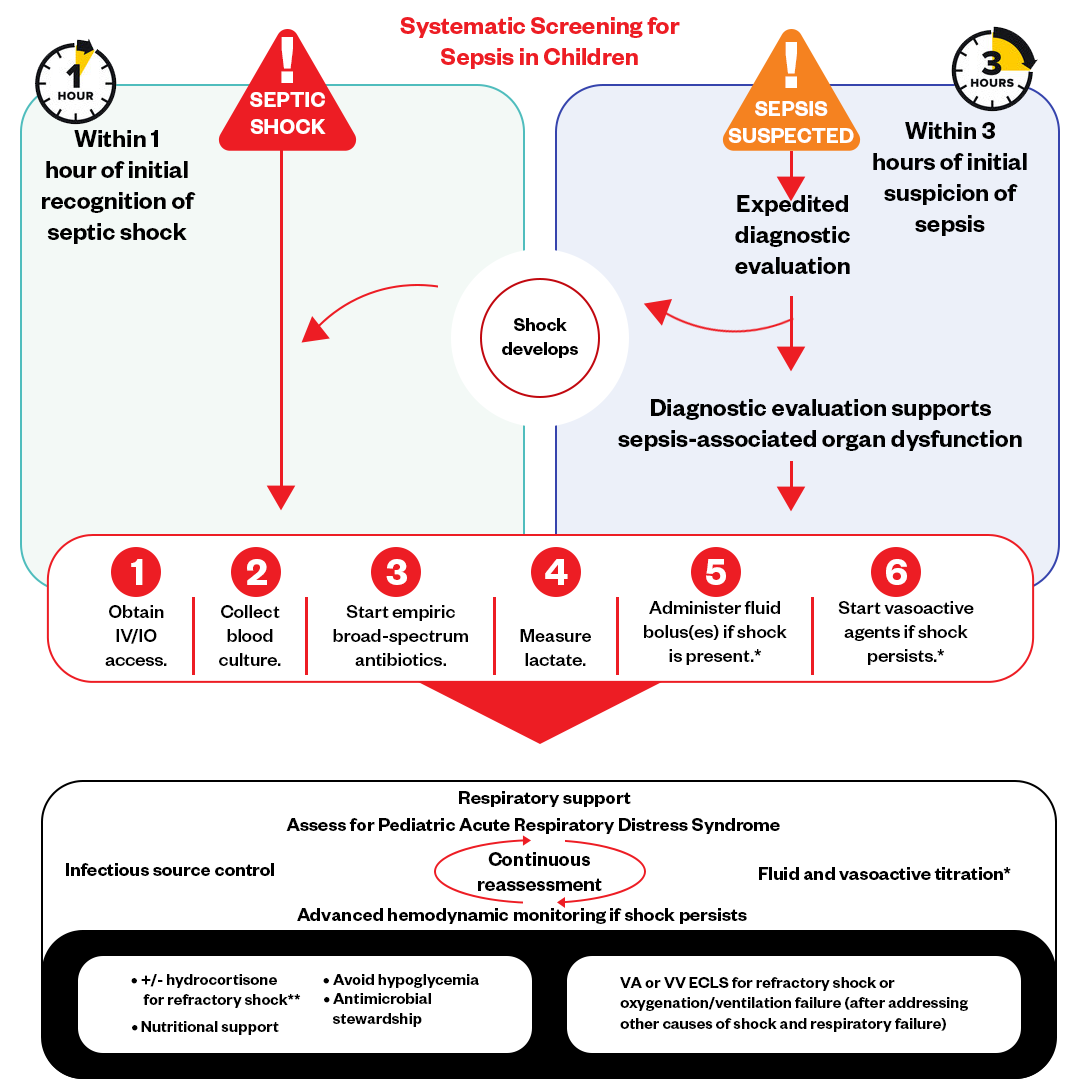
Pediatric Septic Shock Algorithm
Pediatric septic shock refers to a life-threatening condition caused by overwhelming infection leading to cardiovascular dysfunction, cellular metabolic abnormalities, and ultimately multi-organ failure.
The pediatric septic shock algorithm emphasizes early recognition and interventions within 1 hour, including:
1.Early administration of broad-spectrum antibiotics after blood cultures.
2.Rapid administration of isotonic crystalloids (typically 20 mL/kg boluses) to restore circulating blood volume and improve perfusion.
3.Initiation of vasoactive medications (dopamine, epinephrine) for fluid refractory shock to help maintain blood pressure.
4.Management of respiratory and metabolic abnormalities like supplemental oxygen, mechanical ventilation if needed, and correcting glucose/electrolyte levels.
5.Identification of the infection source with imaging cultures so source control interventions can be implemented as soon as possible.
6.Goal-directed therapy - optimize blood pressure for age, normalize lactate and capillary refill, and ensure adequate urine output. Reassess for signs of fluid overload before each bolus.
Close monitoring of vital signs, cardiopulmonary status, perfusion indicators like lactate clearance, and markers of end-organ dysfunction guide ongoing resuscitation efforts. The priority is early, aggressive shock reversal to reduce morbidity and mortality.
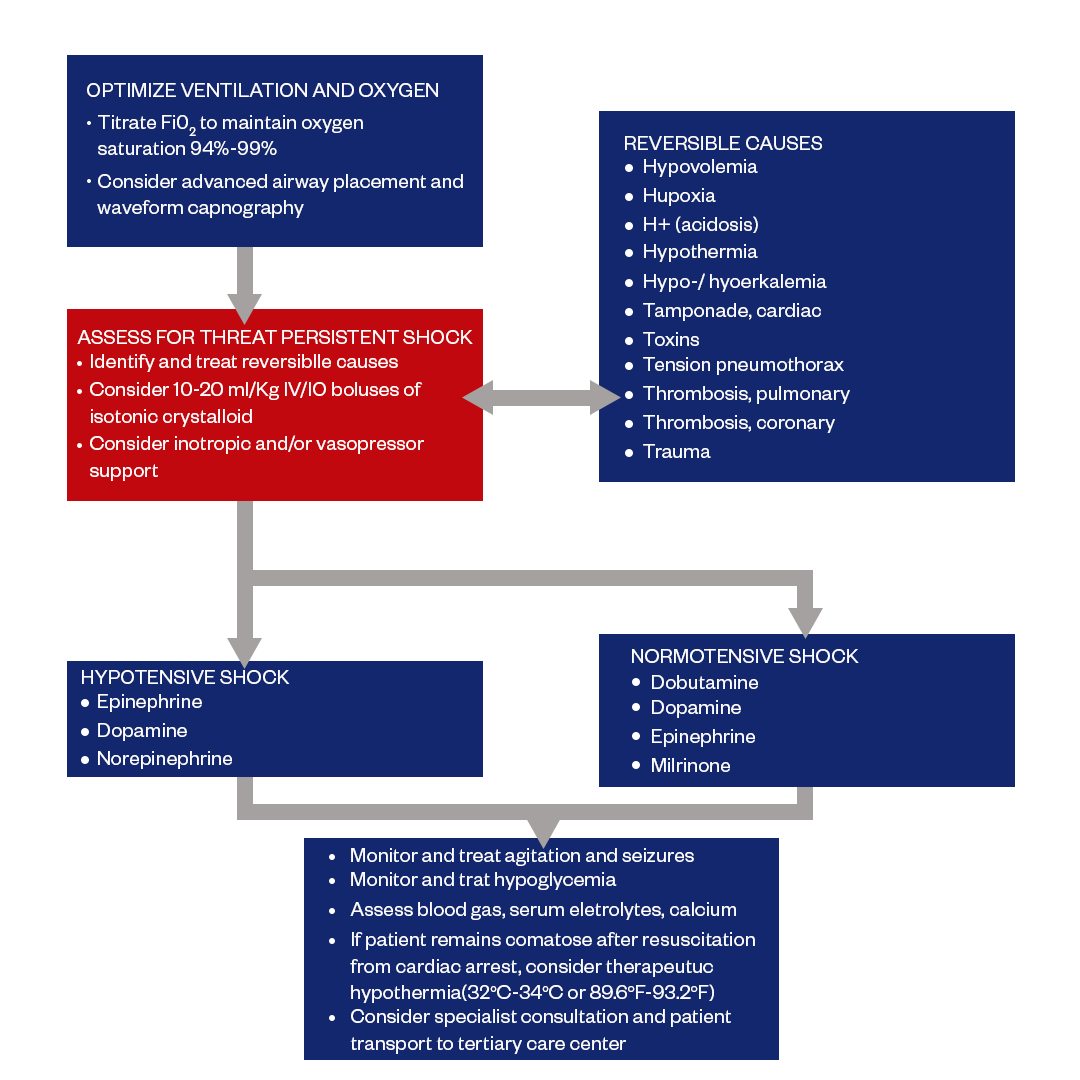
Pediatric Post-Resuscitation Care
Pediatric post-resuscitation care refers to the management of children after the return of spontaneous circulation (ROSC) following cardiac arrest. The goal is mitigating post-cardiac arrest syndrome comprising anoxic brain injury, myocardial dysfunction, systemic ischemia/reperfusion response, and the underlying etiology.
The pediatric post-resuscitation care algorithm emphasizes monitoring neurological and cardiopulmonary status closely, optimizing oxygenation and ventilation, maintaining perfusion with IV fluids and vasoactive infusions, controlling glucose, and preventing hyperthermia. It also includes treating seizures and secondary brain injury, plus early reperfusion if the arrest had a circulatory etiology.
Additional aspects involve gradual withdrawal of life support if there is no improvement despite maximal care, family counseling throughout, and planning-focused rehabilitation if the child survives. Overall, the structured algorithm guides the multidisciplinary care of resuscitated pediatric cardiac arrest patients to facilitate convalescence and recovery.
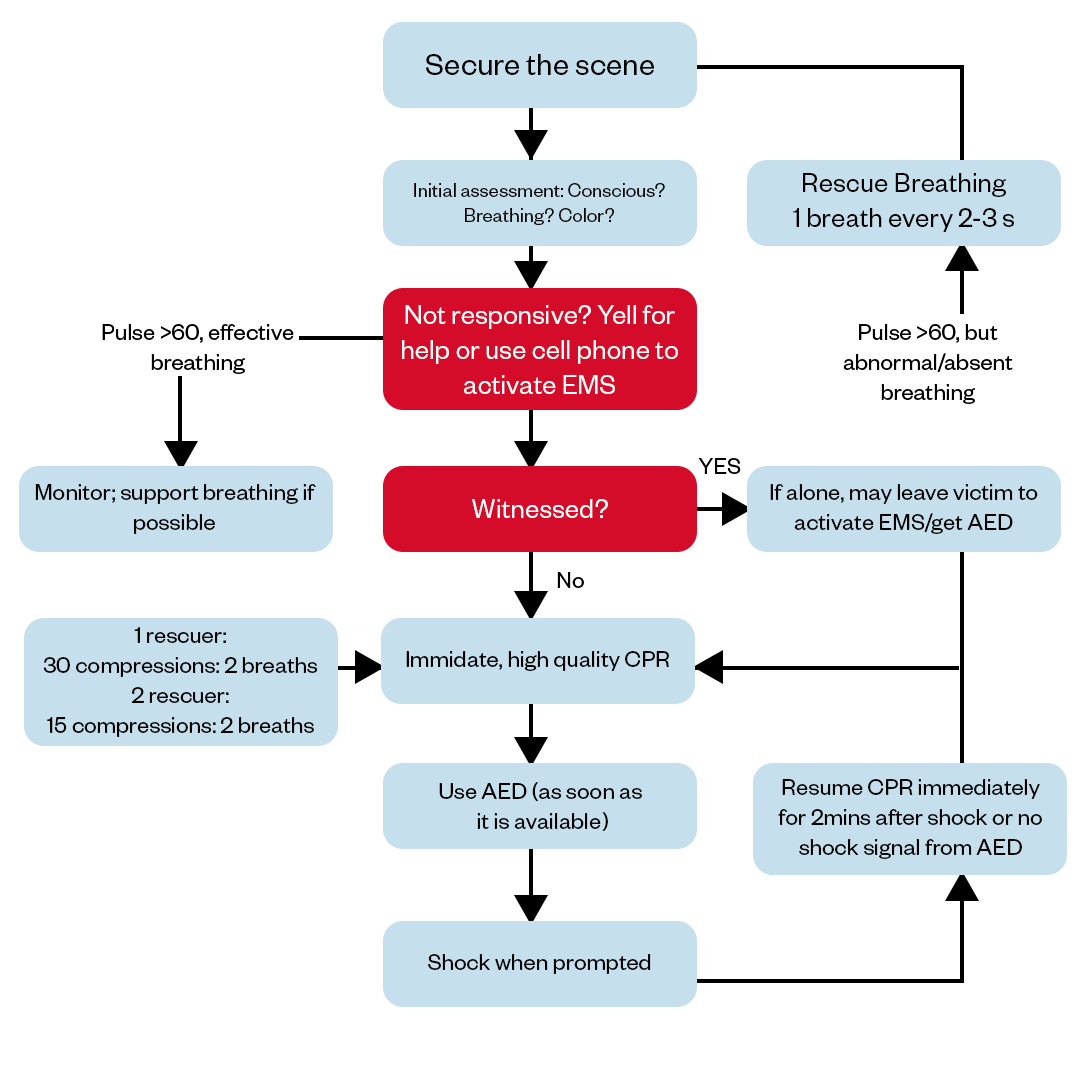
Pediatric BLS Algorithm
The pediatric basic life support (BLS) algorithm provides a standardized approach for healthcare providers to perform cardiopulmonary resuscitation (CPR) in infants and children under cardiac arrest. It aims to establish the return of spontaneous circulation through prompt initiation of high-quality chest compressions along with rescue breaths.
Key steps include rapidly checking responsiveness, calling for help, opening the airway, providing initial ventilations if indicated, and beginning chest compressions at rate of 100-120 per minute with a depth of a third of the anterior-posterior chest diameter while allowing full recoil between compressions.
Ventilations and compressions are coordinated in cycles of a 15:2 ratio for 2 rescuers or 30:2 with a lone rescuer. Once the AED is brought, it is to be attached to allow analysis of heart rhythm and delivery of a shock if indicated, while CPR cycles resume promptly after each attempt. The priority remains on continuous, uninterrupted compressions except if defibrillation is required or to allow pulse checks.
Hypotension
Hypotension, or abnormally low blood pressure, is a key vital sign abnormality monitored in PALS as it reflects shock and inadequate end-organ perfusion. Identifying and properly managing hypotension is vital for reversing shock and preventing subsequent organ damage.
- Assess and continuously monitor blood pressure - hypotension is defined as systolic BP <70mmHg in infants or <70 + (2x age in years) for children 1-10 years old.
- Treat underlying causes of shock if evident (e.g. hypovolemia, sepsis).
- Give 20mL/kg fluid bolus over 5-10 minutes and reassess. Continue boluses PRN to improve BP and clinical markers of perfusion.
- If hypotension persists, consider vasoactive infusions like dopamine or epinephrine.
Hemodynamics
Hemodynamic monitoring involves analyzing cardiovascular variables like heart rate, cardiac output, oxygen delivery, and systemic vascular resistance to gauge the circulatory status and guide shock resuscitation methods.
- Continuously monitor heart rate and assess clinical indicators of perfusion like capillary refill, mental status, pulses, and extremity temperature.
- Target heart rate limits are 60-200bpm for infants and 60-180bpm for children.
- Monitor cardiac rhythm for arrhythmias that may need treatment.
Airway, Breathing, Circulation, and Differential Diagnosis
The ABCs represent the basic assessment and interventions for stabilization - evaluating and establishing a pediatric patient's airway, ensuring adequate oxygenation and ventilation, and supporting circulation. Prioritizing the ABCs is fundamental in pediatric resuscitation.
- Assess airway patency and protect the airway through positioning, suction, and adjuncts like OP or NP airways. Intubate if necessary.
- Ensure adequate oxygenation and ventilation. O2 via nasal cannula, facemask or advanced airway at 100% FiO2. Assist ventilations with BVM if needed.
- Assess circulation with BP, cap refill, pulses, and mentation. Give fluids and/or drugs for hypotension.
Differential Diagnosis
Generating a broad differential diagnosis list based on the clinical presentation is crucial for determining the likely underlying cause of cardiorespiratory instability and customizing therapeutic measures accordingly.
Advanced Airways
For children requiring prolonged ventilatory assistance who do not show improvement with initial basic airway maneuvers, establishing an advanced airway, such as through intubation, facilitates oxygenation and ventilation.
Defibrillation
Defibrillation, or delivery of electrical current to stop life-threatening arrhythmias using an automatic external defibrillator (AED), helps restore organized electrical activity critical for myocardial contractions and cardiac output. Timely defibrillation is life-saving in pediatric shockable rhythms.
- Attach the defibrillator as quickly as possible if profound bradycardia, no perfusing rhythm, or ventricular arrhythmias on the monitor.
- If ventricular fibrillation or pulseless ventricular tachycardia - defibrillate at 2 J/kg. Escalate dose PRN.
- For unstable SVT with poor perfusion - synchronized cardioversion at 0.5-1 J/kg, then increase the dose.
PALS Vital Signs
Normal ranges of a child's vital organs help determine stability versus pathology in pediatric patients based on age and should be continually reassessed. Abnormal vital signs in children can reflect decompensation, so awareness of normal ranges and monitoring trends is a critical component of PALS protocol and decision-making.
Heart Rate
The heart rate reflects the frequency of cardiac contractions and systemic perfusion. The pediatric resuscitation algorithm follows to manage the heart rate of pediatric patient to the normal, while the normal heart rate range varies by age:
Newborns (0-3 months): 100-180 beats per minute
Infants (3 months - 2 years): 100-180 bpm
Children (2-10 years): 60-140 bpm
Children over 10 years: 60-100 bpm
Respiratory Rate
The respiratory rate indicates the frequency of respiratory cycles per minute and the PALS protocol guides the management of pediatric patients' respiration. Normal respiratory rate by age:
Newborns: 30-60 breaths per minute
Infants: 25-50 breaths per minute
Children (2-5 years): 25-30 breaths per minute
Children (5 years+): 15-20 breaths per minute
Blood Pressure
Normal BP varies substantially based on a child's height and age. Hypotension risk thresholds correlate with patient age, weight, and clinical context. For example:
- A 6-month-old with an SBP < 70 mm Hg would be considered hypotensive.
- The treatment target would be to achieve an SBP >60 mm Hg through the administration of fluid boluses and/or vasoactive medications.
- An 8 years old child will be considered hypotensive if their SBP drops below 86 mm Hg (70 + (2 x 8) years).
- The post-resuscitation BP goal for this 8 years old would be ≥ 90 mm Hg systolic.
Oxygen Saturation
Oxygen saturation or SpO2 (%) reflects the amount of hemoglobin bound to oxygen in the arterial circulation. Normal SpO2 is > 94% at room air across pediatric age groups. Cyanosis may be present when saturation is <90%. Hypoxemia or insufficient oxygenation manifests with lower saturations.
Temperature
Core body temperature is maintained within a narrow range. Normal temperature in children is 36-38°C or 96.8-100.4°F. Hypothermia (temp <36°C) increases mortality risk and complicates resuscitation. The PALS Algorithm includes an assessment for temperature abnormalities to promptly address and manage such conditions. Hyperthermia (temp >38.5°C) may reflect infection, neurological dysfunction, or heat exposure.
PALS Algorithm FAQs
Who needs PALS?
Any medical professional who provides frontline care for vital pediatric cases should pursue PALS certification and must know PALS algorithm effectively. The protocols cover crucial interventions to help save children's lives in emergency situations. Pediatric Advanced Life Support (PALS) training is most relevant for healthcare providers who regularly treat critically ill or injured children. This includes pediatricians, ER physician, nurses, paramedics and EMTs, respiratory therapists, and any other medical professionals responsible for stabilizing injured children.
What is the systematic approach algorithm in PALS?
The PALS systematic approach algorithm provides a structured framework for assessing and managing critically ill or injured children. The pediatric systematic approach enables providers to rapidly identify and respond to life threats, resuscitate if necessary, uncover underlying issues, and continually reassess to optimize management. Key aspects of PALS systematic approach algorithm include:
Primary Assessment:
- Initial impression - quickly identifying life threats
- Level of consciousness - AVPU scale
- Airway - open and maintainable
- Breathing - rate, work of breathing, oxygenation
- Circulation - heart rate, skin perfusion, capillary refill
- Disability - neurological status
Resuscitation:
- Following Pediatric Basic Life Support steps if needed - airway, breathing, circulation
- Administering medications/fluids per PALS pharmacotherapy protocols
Secondary Assessment:
- Head-to-toe exam for additional injuries once child is stabilized
- Review of systems to uncover any underlying conditions
- Checking vital signs and oxygenation status
Integration:
- Integrating all findings from primary and secondary surveys
- Identifying working diagnosis and priorities for management plan
- Providing stabilizing interventions, treatment, and supports
Reassessment:
- Frequently reassessing patient and effectiveness of interventions
- Modifying plan accordingly
What is the ABCDE approach in PALS algorithm?
The ABCDE approach in PALS algorithm stands for Airway, Breathing, Circulation, Disability, and Exposure/Environment. It guides providers to first assess and intervene on threats to airway patency, oxygenation/ventilation, circulatory inadequacy, neurological disability, and exposure issues. This systematic method facilitates rapid identification of problems that can imminently lead to cardiopulmonary arrest so providers can quickly mitigate life threats and resuscitate pediatric patients exhibiting respiratory failure, shock, or neurological deterioration.
How do you assess a child's progress?
Ongoing assessment and reevaluation of the child's condition determines if the PALS protocol is successfully improving cardiopulmonary and neurological function to guide appropriate adjustments in care. There are a few key ways to assess a child's progress in the Pediatric Advanced Life Support (PALS) protocol:
- Reassess vital signs - This includes heart rate, blood pressure, temperature, oxygen saturation, and respiratory rate. Improving vital signs can indicate the child is responding well to interventions.
- Check cardiopulmonary status - Lung sounds, capillary refill time, and pulse quality provide information on oxygenation and perfusion. Improvement suggests circulatory and respiratory function are adequate.
- Note neurological status - Level of consciousness, pupil reaction, and movements give insight on neurological function. A child that is more alert and responsive is showing positive progress.
- Review laboratory results - Trends in blood gas values, lactate, blood counts, etc. provide objective data about the child's metabolic status. Normalizing labs are reassuring.
- Ensure interventions are effective - Monitor how well medications, fluids, and other treatments are working to stabilize the patient. Discontinue or modify ineffective interventions.
- Repeat primary and secondary surveys - Serial exams uncover any new or evolving problems to address.
What is the difference between NRP and PALS?
The NRP program focuses specifically on newborns, addressing their unique critical care needs in the all-important initial minutes and hours after birth. Its protocols cover resuscitation, assessment, and stabilization interventions focused to the physiology and typical emergency presentations of neonates.
In contrast, PALS systematic approach algorithm applies to older infants, children, and adolescents, concentrating on anatomy, pathology, illnesses, and injuries relevant from 1 year of age through young adulthood. So while both involve pediatric life support principles, NRP zooms in on the newborn period alone with neonatal-specific training, while PALS covers later childhood problems requiring age-appropriate acute management approaches.

Owner Jeff Haughy has been providing high-quality care in the EMS industry since 1995 and started his Fire Service career with the Alameda Fire Department in 1991 as a Fire Explorer.