Adult Suspected Stroke Algorithm
The ACLS Suspected Stoke Algorithm is a part of the Advance Cardiac Life Support (ACLS) algorithm used in emergency medicine to manage patients with acute stroke. A stroke occurs when the blood supply to part of the brain is blocked, leading to the death of brain tissue. The American Heart Association (AHA) provides guidelines for Advanced Cardiovascular Life Support (ACLS), which includes specific algorithms for managing various cardiac and respiratory emergencies, including stroke.
Identifying the Types of Acute Stroke
The two types of acute stroke are listed below, they have their own cause, symptoms, risk factors, and treatments. Recognition of the stroke types is crucial for determining the most appropriate treatment.
Ischemic Stroke
The ischemic stroke is the most common stroke accounting for almost 85% of patients. The stroke is caused by a blood clot or an embolus (a clot traveling from another part of the body) that blocks a blood vessel in the brain, causing reduced blood flow and oxygen flow to brain tissue.
To identify ischemic stroke, providers should look for sudden onset of neurological deficits like unilateral weakness, speech impairment, or vision loss. Risk factors like atrial fibrillation, carotid stenosis, and hypertension may raise suspicion. Diagnostic tests like CT or MRI can confirm occlusion of a cerebral artery.
The leading cause of ischemic stroke is atherosclerosis, where fatty deposits build up on the inside walls of the blood vessels, leading to the formation of plaques or atheromas.
Ischemic Stroke Treatment:
Intravenous thrombolytic therapy, also known as fibrinolytic therapy, is the mainstay of acute ischemic stroke treatment if given within 3-4.5 hours of symptom onset. It involves drugs like tissue plasminogen activator (tPA) that dissolve blood clots to restore blood flow and oxygen to the brain.
Fibrinolytic therapy should be considered for patients presenting within the treatment window with disabling neurological deficits but no contraindications like recent surgery, bleeding disorders, or anticoagulant use. Time is brain, so rapid assessment and administration of fibrinolytics is crucial to avoid the brain injury. Endovascular thrombectomy is also an option within 6-24 hours for proximal large vessel occlusions not responding to fibrinolytics.
Treatment focuses on quickly restoring perfusion to salvage threatened brain tissue. Providers should act swiftly in accordance to the adult stroke algorithmic approach when ischemic stroke is suspected to minimize permanent damage.
Hemorrhagic Stroke
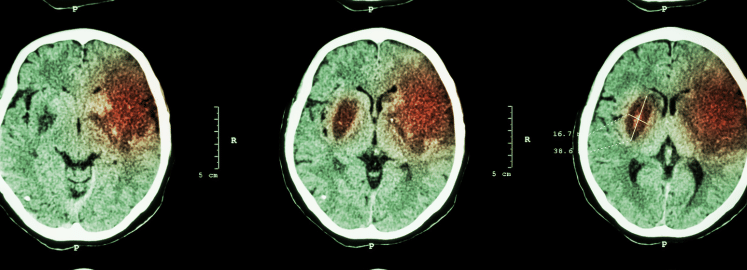
This hemorrhagic stroke is caused when blood vessels in the brain rupture, causing internal bleeding in the brain areas.
The hemorrhagic stroke makes up about 15% of all stroke cases. There are two types of hemorrhagic strokes: intracerebral hemorrhage (bleeding within the brain) and subarachnoid hemorrhage (bleeding in the space around the brain).
To identify it, providers should look for sudden severe headache, vomiting, altered mental status, and neurological deficits like hemiparesis. Risk factors include hypertension, anticoagulant use, aneurysms, and AVMs. Diagnostic tests like CT or MRI can visualize the hemorrhage and distinguish between intracerebral and subarachnoid types.
Treating Hemorrhagic Stroke:
While the initial intervention should be administered in a processed way. The treatment focuses on stabilizing vital signs and reducing intracranial pressure. Surgery may be needed to evacuate large hematomas or repair ruptured aneurysms. Preventing rebleeding and vasospasm are also important in subarachnoid hemorrhage. Providers should monitor for hydrocephalus and manage blood pressure to prevent further bleeding. The main goals are controlling intracranial pressure and preventing another hemorrhage.
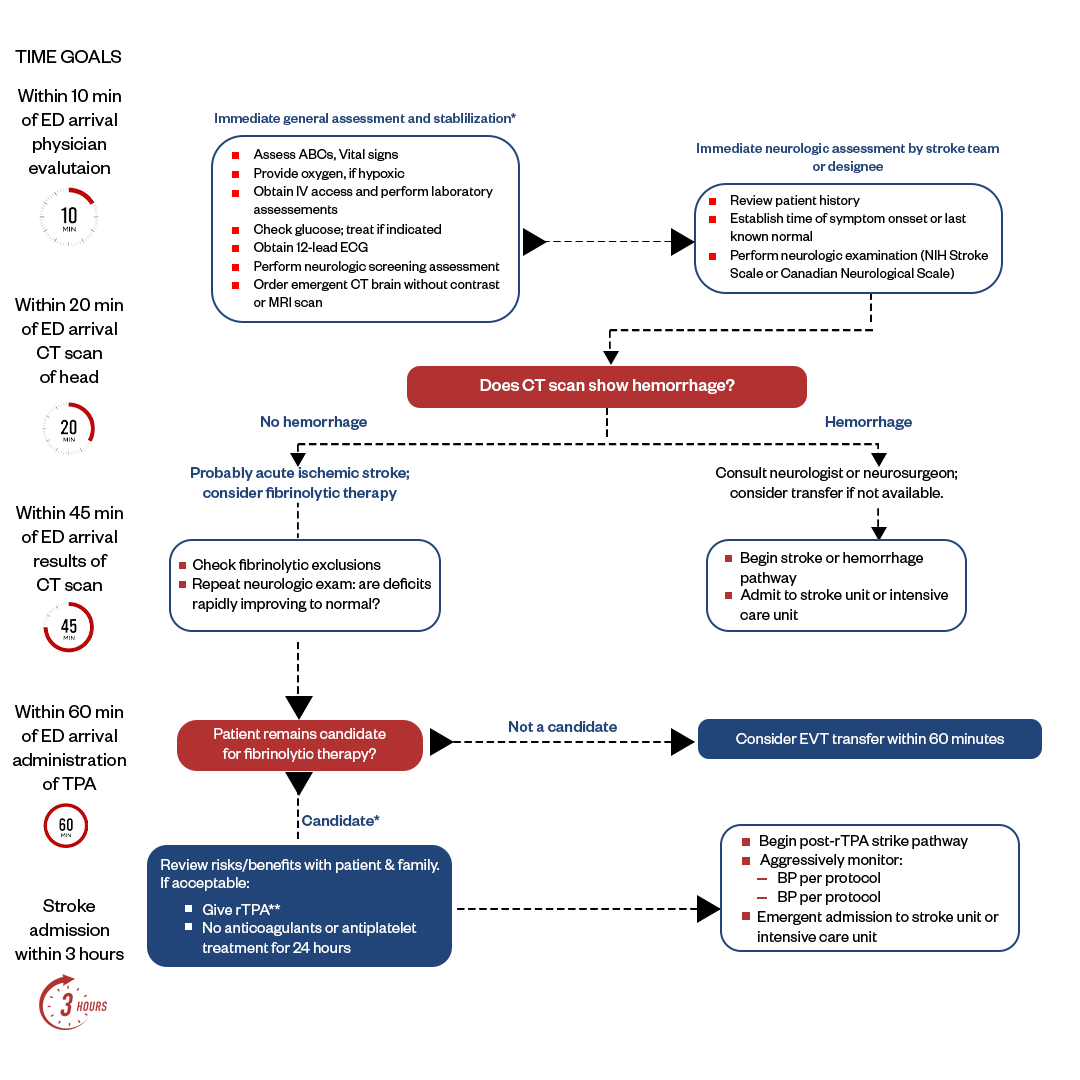
Suspected Stroke Treatment Algorithm
Stroke treatment follows a rapid ACLS stroke algorithm to provide time-sensitive interventions that can significantly improve outcomes. Initial stroke assessment via physical exam and imaging determines the type of stroke - ischemic or hemorrhagic. ACLS stroke protocol is initiated with supportive care. For ischemic strokes, treatment follows an algorithm to quickly determine eligibility for intravenous thrombolysis or endovascular thrombectomy reperfusion therapy. Hemorrhagic strokes are managed with medications, interventions to control bleeding, and neurosurgical evaluation. Regardless of stroke type, treatment also focuses on preventing complications and initiating early rehabilitation to maximize recovery. The speed and coordinated action of the stroke treatment algorithm gives patients the best chance for survival and reduced disability. The systematic approach for an acute stroke algorithm is as follows:
Recognition of Stroke Symptoms
First, recognize potential stroke symptoms, including sudden numbness or weakness in the face, arm, or leg (especially on one side of the body), sudden confusion, trouble speaking or understanding speech, sudden severe headache, and difficulty walking or maintaining balance.
Activation of Stroke Team
If the stroke is suspected, a stroke alert or code stroke activates a specialized stroke team. This team typically includes neurologists, emergency department staff, and radiology personnel.
Rapid Assessment
The patient's vital signs are assessed, and a thorough medical history is obtained, including the time of symptom onset. The onset time is crucial, as it helps determine eligibility for time-sensitive treatments like thrombolytic therapy.
Neurological Examination
A detailed neurological examination assesses the patient's motor and sensory functions, coordination, speech, and other neurological signs. The National Institutes of Health Stroke Scale (NIHSS) may be used to quantify the severity of stroke symptoms.
Imaging Studies
An urgent brain imaging study, typically a non-contrast CT scan, is performed to distinguish between ischemic and hemorrhagic strokes. This helps guide treatment decisions.
Laboratory Tests
Blood tests, such as a complete blood count (CBC), coagulation studies, and blood glucose levels, are checked to rule out other potential causes of stroke-like symptoms and to assess eligibility for specific treatments.
Thrombolytic Therapy (If Indicated)
If an ischemic stroke is confirmed and the patient meets specific criteria, thrombolytic therapy with a medication like tissue plasminogen activator (tPA) may dissolve the blood clot and restore blood flow to the brain. Timing is crucial; this treatment is typically given within a specific time window from symptom onset.
Blood Pressure Management
Blood pressure is monitored and managed to maintain appropriate levels, balancing the need for adequate cerebral perfusion with the risk of hemorrhagic transformation (bleeding into the brain) after thrombolytic therapy.
Secondary Prevention and Evaluation
After initial stabilization and treatment, further evaluation is conducted to identify the underlying cause of the acute stroke and to implement secondary prevention strategies. This may include imaging of blood vessels (e.g., CT angiography, MR angiography) and additional tests to assess cardiac function and rhythm.
Rehabilitation and Follow-Up
Stroke rehabilitation and ongoing medical management are essential components of care to promote recovery and reduce the risk of recurrent strokes.
Critical Periods from Hospital Arrival
- Door-to-imaging time: Getting a CT or MRI scan quickly is critical to determine if a patient is having an ischemic stroke (caused by a clot) or a hemorrhagic stroke (caused by bleeding). Guidelines recommend brain imaging within 25 minutes of hospital arrival.
- Door-to-needle time: For ischemic strokes, the most effective treatment is intravenous thrombolysis (clot-busting medication) as soon as possible after onset of symptoms. Guidelines recommend administering IV tPA within 60 minutes of hospital arrival.
- Door-to-groin time: For large vessel ischemic strokes, endovascular thrombectomy (physically removing the clot) has become the standard of care. Guidelines recommend the procedure be performed within 90 minutes of hospital arrival for best outcomes.
- LVO stroke identification: Identifying a suspected large vessel occlusion (LVO) stroke right away using a clinical screening tool can help fast-track the patient for thrombectomy.
- Transfer times: For patients who arrive initially at a primary stroke center, rapid transfer to a comprehensive stroke center for thrombectomy is important. Target times are within 3 hours of onset of symptoms.
Secondary Prevention and Evaluation for Adult Acute Stroke
- Within 24 hours: Complete a full stroke workup including lab tests, EKG, vascular imaging etc. to determine the cause of stroke and plan secondary prevention.
- Within 48 hours: Initiate treatments to prevent recurrence e.g. antiplatelets, anticoagulants, statins, blood pressure control.
- Before discharge: Assess for dysphagia to reduce aspiration risk. Begin education about lifestyle changes to reduce risk factors.
Rehabilitation Initiation
- Within 24-48 hours: Perform early rehab evaluation including PT, OT, speech therapy. Begin mobilizing patient.
- During hospitalization: Provide daily rehab interventions. Determine appropriate rehab needs at discharge.
- Before discharge: Train and educate caregivers for post-stroke needs.
Disposition Planning
- Within 24-48 hours: Determine appropriate discharge destination e.g. home vs. rehab facility.
- If going home: Begin coordinating home health services based on needs.
- If going to rehab: Finalize transfer within 7 days and communicate with facility about patient care needs.
- Before discharge: Confirm all equipment, medications, outpatient therapy arrangements are in place for a safe discharge.
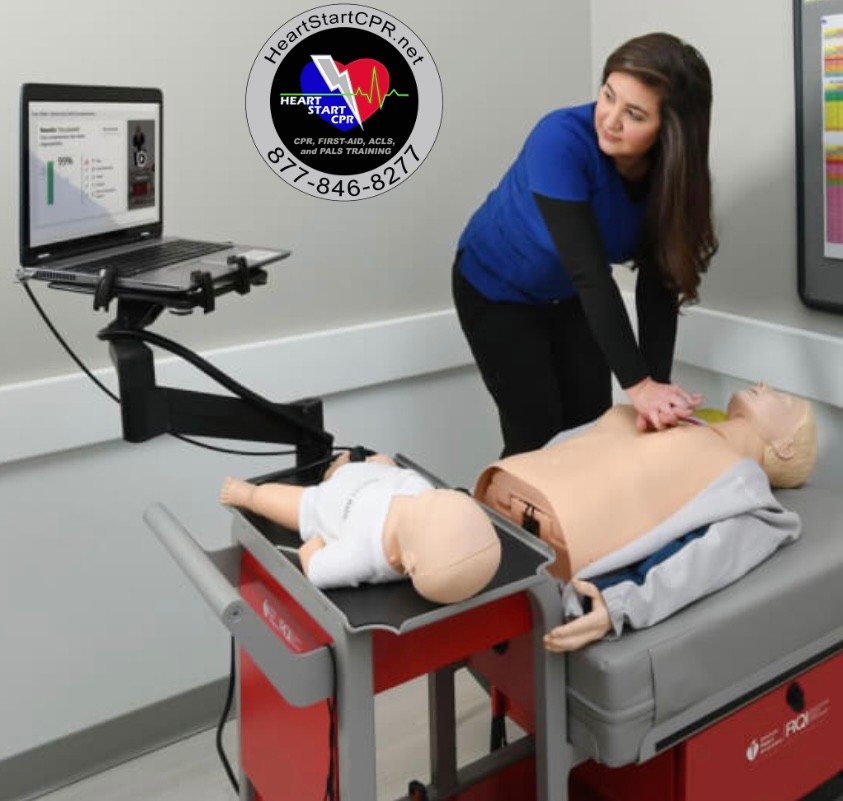
Fast and Convenient
Take ACLS Classes
*Nationally Accepted
ACLS
CERTIFICATION
AHA ACLS course
State-of-the-Art Facilities
Unlimited Exam Retakes
$260
ACLS
ONLINE CERTIFICATION
AHA ACLS Online Course
100% online training
Unlimited Exam Retakes
$280
FAQs of Suspected Stroke Algorithm
What are the steps for a suspected stroke?
Recognition of stroke symptoms, activation of atroke team, rapid assessment, neurological examination, imaging studies, laboratory tests, blood pressure management, and secondary prevention and evaluation are the steps for a suspected stroke algorithm.
What is the first critical decision point in the suspected stroke algorithm?
The first critical decision point in the suspected stroke algorithm is typically to assess if the patient is experiencing any life-threatening issues or require any emergency attention. Focus on patient’s ABCs (Airway, Breathing and Circulation).
What are the 5 silent signs of a stroke?
The 5 symptoms of silent stroke are:
- Memory problems or cognitive decline
- Changes in mood or personality
- Difficulty with coordination or balance
- Mild weakness in a limb
- Visual changes or visual disturbances
What are the 8 Ds of stroke in ACLS?
The 8 Ds of stroke in ACLS are detection (D1), dispatch (D2), delivery (D3), door (D4), data (D5), decision (D6), drug/device (D7), and disposition (D8).
What are the ABCs of stroke treatment?
The ABCs in stroke treatment or ACLS are Airway, Breath, and Circulation. It’s a simplified way of remembering key components of initial care for a stroke patient. Theses components help healthcare providers assess and address critical aspects of stoke management.
What is the golden hour of a stroke?
The first 60 minutes after the stroke is considered to be the golden hour of a stroke. There is huge chance of saving a patient if suspected and received immediate emergency help within the golden hour.
What is the FAST mnemonic for stroke?
The FAST mnemonic is a simple and common ways to remember the symptoms and signs of stroke. FAST stands for Face, Arm, Speech,Time. Meaning look for any sudden weakness or drooping on one side of the face, check if the victim can raise their both arms, listen if they have trouble speaking, and lastly its time to call the emergency help, call 911.

Owner Jeff Haughy has been providing high-quality care in the EMS industry since 1995 and started his Fire Service career with the Alameda Fire Department in 1991 as a Fire Explorer.