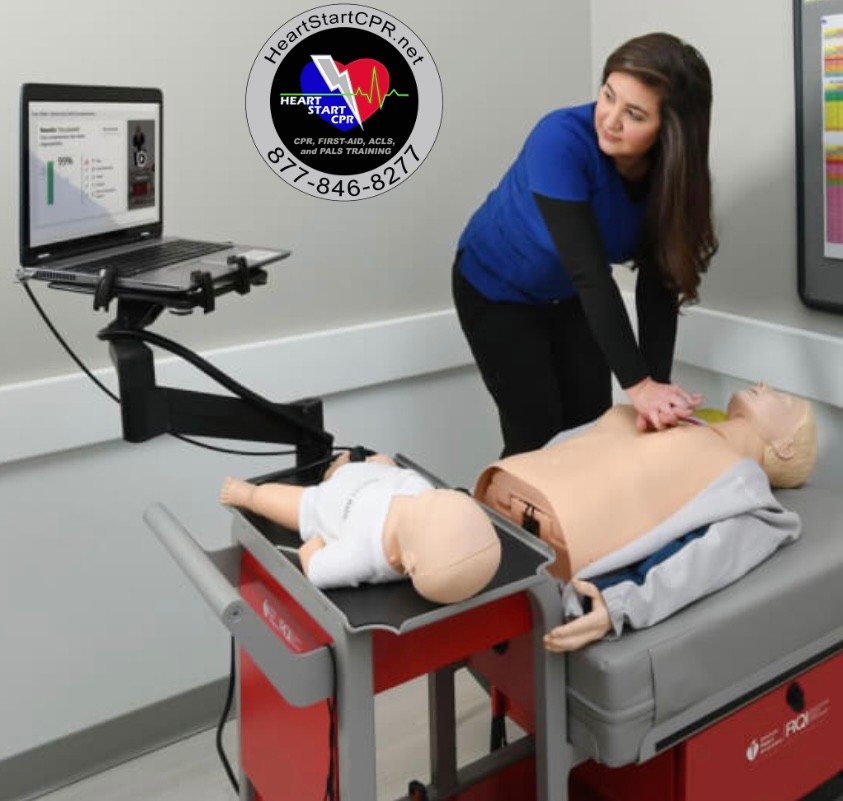
Tachycardia ACLS Algorithm
Usually, the heart beats at the rate of 60 - 100 times per minute while at rest. When the heartbeat rate exceeds the normal and consistently exceeds 100 beats per minute, the condition is considered tachycardia. The ACLS Tachycardia Algorithm is a part of the Advance Cardiac Life Support (ACLS) algorithm used in emergency medicine to manage patients with fast heartbeat.
A variety of factors, both physiological and pathological, can cause tachycardia. To name some conditions - fever, shock, medication, stress, hypoxemia, etc., can cause a high heartbeat.
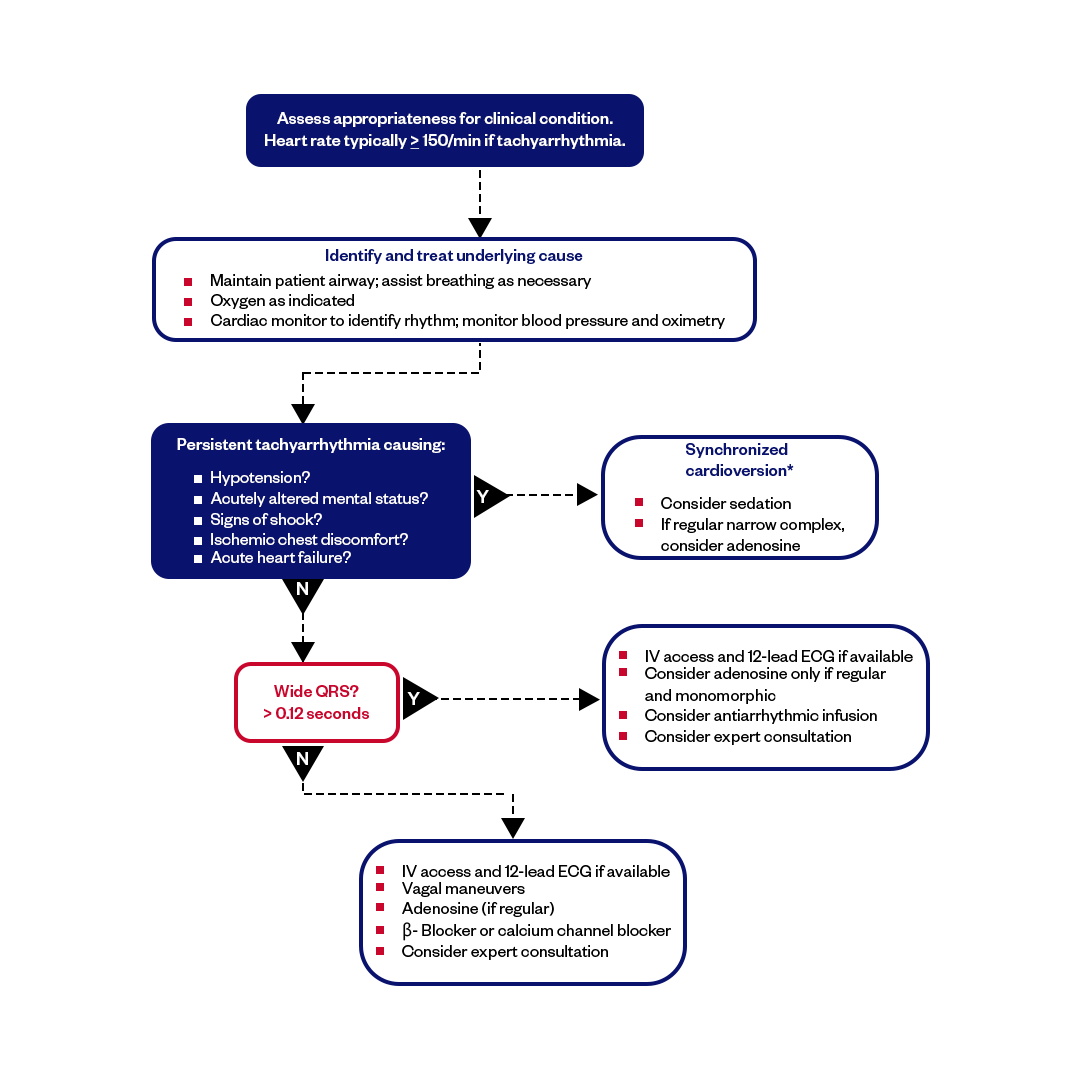
Image: Tachycardia With a Pulse Algorithm
Signs and Symptoms of Tachycardia
Heart pounding, sensation of race, chest pain, fainting, and rapid pulse rate are some of the symptoms of tachycardia. But, symptoms are rare when your heart rate is somewhere between 100 to 150 bpm. The higher the heartbeat rate, it’s more likely the symptoms of tachycardia. In this situation conducting thorough research can help assess the patient’s state.
Tachycardia Treatment Algorithm
The treatment for tachycardia depends on the specific type and underlying cause of the condition and the severity of symptoms. But before the medication or any treatment, immediately identifying the cause helps you better assess a stable patient with tachycardia ACL treatment. Here are the step-by-step approach of ACLS tachycardia algorithm that a rescuer should follow:
- Assess the Patient
- Obtain a 12-lead ECG
- Determine the Tachycardia Type
- Assess Vital Signs
- Consider Underlying Causes
- Vagal Maneuvers
- Administer Medications
- Synchronized Cardioversion
- Monitor Continuously
The Treatments in ACLS Tachycardia Algorithm for a patient experiencing different tachycardia are as follows:
Supraventricular Tachycardias (SVT):
Vagal Maneuvers: Attempt vagal maneuvers like the Valsalva maneuver, carotid sinus massage, or cold stimulus to the face.
Adenosine: Administer adenosine as a rapid intravenous (IV) bolus. It's often the first-line medication for SVT.
Beta-Blockers or Calcium Channel Blockers: In stable cases, oral or IV beta-blockers (e.g., metoprolol) or calcium channel blockers (e.g., diltiazem) may be used.
Atrial Fibrillation (AF) and Atrial Flutter:
Rate Control: Use medications such as beta-blockers, calcium channel blockers, or digoxin to control heart rate.
Rhythm Control: Administer anti-arrhythmic medications like amiodarone or flecainide to restore and maintain normal sinus rhythm.
Anticoagulation: Consider anticoagulant therapy to prevent thromboembolic events in patients with AF at risk.
Ventricular Tachycardia (VT):
Stable VT: Administer anti-arrhythmic drugs like amiodarone or lidocaine.
Unstable VT: Perform synchronized cardioversion using appropriate energy levels.
Consider Magnesium: Consider IV magnesium sulfate in cases of torsades de pointes or suspected magnesium deficiency.
Wide-Complex Tachycardia of Unknown Origin:
Stable Wide-Complex Tachycardia: For stable WCT with a wide QRS complex, administer IV amiodarone.
Unstable Wide-Complex Tachycardia: Perform immediate synchronized cardioversion.
Sinus Tachycardia:
Identify and Treat Underlying Cause: Address and manage the underlying condition causing sinus tachycardia, such as pain, fever, or anxiety.
Beta-Blockers: Consider beta-blockers if appropriate for symptom control.
Atrioventricular Nodal Reentrant Tachycardia (AVNRT) and Atrioventricular Reentrant Tachycardia (AVRT):
Vagal Maneuvers: Attempt vagal maneuvers.
Adenosine: Administer adenosine as a rapid IV bolus.
If unsuccessful: Consider other anti-arrhythmic medications or catheter ablation for recurrent episodes.
Wolff-Parkinson-White (WPW) Syndrome:
Procainamide or Amiodarone: Administer procainamide or amiodarone for acute management.
Definitive Treatment: Catheter ablation is often recommended to eliminate the accessory pathway responsible for WPW syndrome.
Note: Specific treatment protocols may vary based on the patient's clinical condition, and healthcare providers must follow current guidelines and individualized patient care plans. Treatment choice depends on the type of tachycardia, the patient's clinical presentation, and any underlying medical conditions.
Medication Doses and Details
Adenosine IV dose:
- Adenosine is administered intravenously in two doses: Initial dose: 6mg rapid IV followed by NS flush
- 2nd dose: 12mg if needed
Procainamide IV dose:
20-50mg/min IV
Synchronized Cardioversion rules:
- QRS narrow and regular: 50-100 J
- QRS narrow and irregular: 120-200 J
- QRS wide and regular: 100 Joules
- QRS wide and irregular: Immediately defibrillate (not synchronized)
Amiodarone IV dose:
150mg over 10 min
Sotalol IV dose:
100mg over 5 minute
Final Thoughts
Understanding ACLS Tachycardia Algorithm and its treatment is important for healthcare providers. A systematic approach based on ACLS protocols, accurate diagnosis, and tailored interventions in managing tachycardia is critical in ensuring better patient outcomes and reducing the risks associated with rapid heartbeat conditions.
Fast and Convenient
Take ACLS Classes
*Nationally Accepted
ACLS
CERTIFICATION
AHA ACLS course
State-of-the-Art Facilities
Unlimited Exam Retakes
$260
ACLS
ONLINE CERTIFICATION
AHA ACLS Online Course
100% online training
Unlimited Exam Retakes
$280
FAQs of ACLS Tachycardia Algorithm
What are the symptoms of tachycardia?
Chest pain, rapid heartbeat, dizziness, breath shortness, fainting, and cardiac arrest are the symptoms of tachycardia.
What is the most common tachycardia?
Atrioventricular Nodal Reentrant Tachycardia (AVNRT) is accounted in over 60% of patients.
What do you do for tachycardia?
Vagal maneuvers can initially be approached to slow down the heartbeat. Coughing and putting an ice pack on your face can help your heart calm down.
How long is too long for tachycardia?
If the tachycardia lasts longer than 30 minutes, you have been diagnosed with SVT. You will experience breath shortness and chest pain. Immediately call 911.
How long can your heart stay in tachycardia?
Tachycardia can last for seconds, minutes, or hours or can be repeated several times within a day. The heart rate in this situation can go up to 250 bpm.
What is the first drug of choice in a tachycardia according ACLS guidelines?
According to ACLS guidelines, the first drug of choice in stable tachycardia with a narrow QRS complex is adenosine, given as a rapid IV push of 6 mg followed by a normal saline flush. If the rhythm is regular and monomorphic, adenosine may also be considered for unstable patients before synchronized cardioversion. Expert consultation should be strongly considered for stable wide QRS complex tachycardia, and antiarrhythmic infusions such as procainamide, amiodarone, or sotalol IV may be used.
What are the non-drug therapies for tachycardia?
Procedures like vagal maneuvers, carotid massage, or Valsalva maneuvers are non-drug therapies used to manage certain types of tachycardia.

Owner Jeff Haughy has been providing high-quality care in the EMS industry since 1995 and started his Fire Service career with the Alameda Fire Department in 1991 as a Fire Explorer.