ACLS Adult Cardiac Arrest Algorithm

The ACLS Cardiac Arrest Algorithm is a set of guidelines used in advanced cardiovascular life support, specifically for managing and treating patients during cardiac arrest events. It is divided into two branches: The left and right branch. The left branch is for the treatment of ventricular fibrillation and pulseless ventricular tachycardia, and the right branch is for the treatment asystole and pulseless electrical activity(PEA).
High-quality CPR is central to the Advanced Cardiovascular Life Support (ACLS) algorithm. Effective chest compressions should reach a depth of at least 2 inches and be administered at a rate of 100-120 compressions per minute, according to the ACLS Cardiac Arrest Algorithm. This combination ensures optimal blood circulation and adequate oxygenation of vital organs. Full chest recoil after each compression is crucial as it ensures the heart is filled with blood, preparing it for the next compression.
The physical demands of continuous cardiopulmonary resuscitation (CPR) necessitate the rotation of the individual, delivering compressions every 2 minutes to prevent fatigue and maintain efficiency. Minimizing interruptions during compressions is of paramount importance in the cardiac arrest algorithm; each pause can substantially reduce perfusion to vital organs.
Ventilation plays a pivotal role in resuscitation, with over-ventilation being a potential hazard. It can increase intrathoracic pressure, hindering venous return and compromising the effectiveness of compressions. The recommended 30:2 compression-to-ventilation ratio, in the absence of an advanced airway, is essential for balancing oxygenation and circulation, as per ACLS cardiac arrrest algorithm.
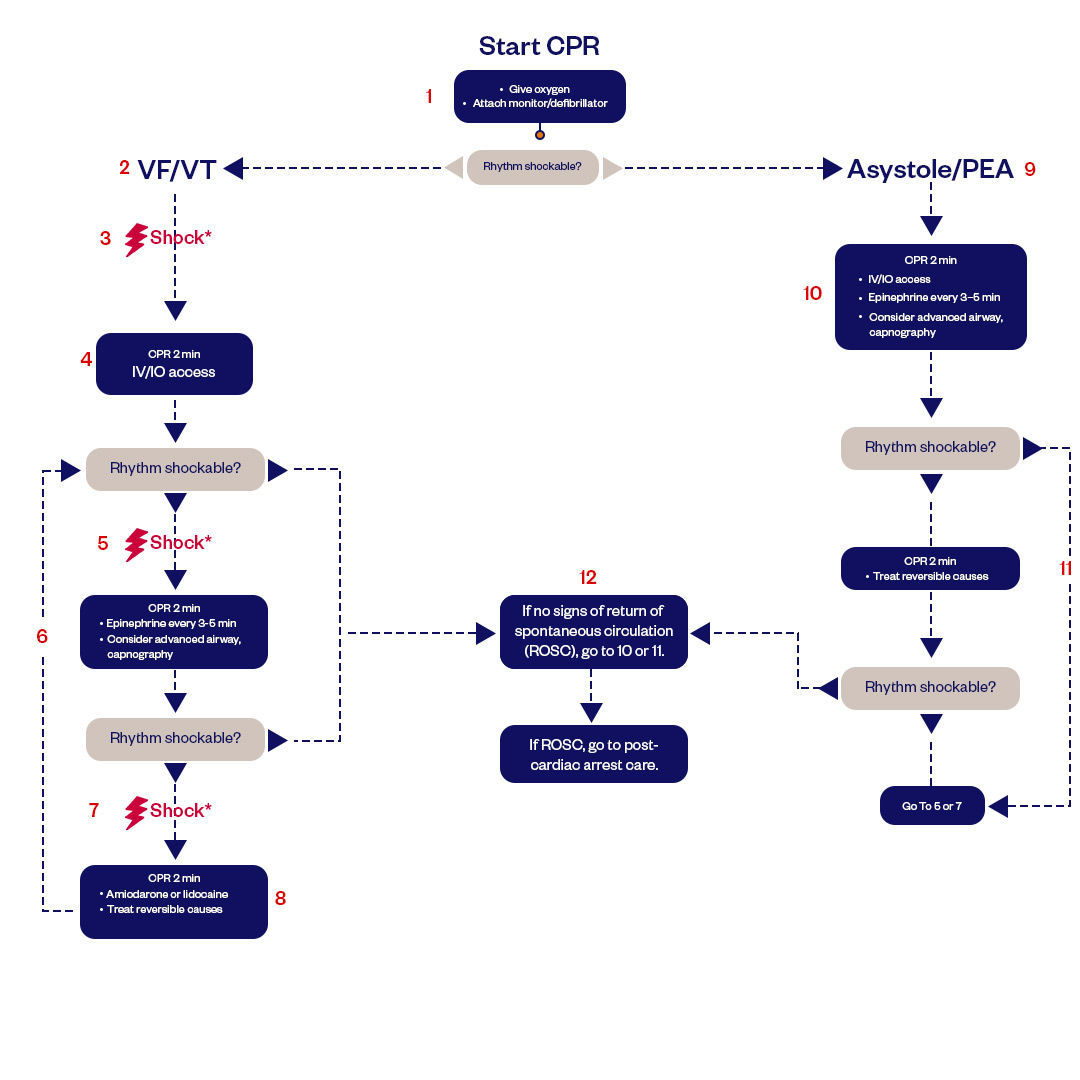
Figure: Adult Cardiac Arrest Algorithm
Cardiac Arrest Algorithmic Approach
The AHA ACLS protocol provides a structured algorithmic approach to managing cardiac arrest. Immediately upon recognizing cardiac arrest, high-quality CPR should be initiated, with chest compressions at a rate of 100-120 per minute and a depth of 2-2.4 inches. Airway management and oxygenation are also priorities, but excessive ventilation should be avoided.
The ACLS cardiac arrest algorithm emphasizes the critical importance of CPR and continuous chest compressions, with interruptions minimized. After delivering CPR for 2 minutes, rhythm analysis using a defibrillator is performed. If a shockable rhythm is detected, a single shock is delivered, continue CPR for 2 minutes, and check rhythm for no more than 10 seconds every 2 minutes. Epinephrine, a significant component in ACLS cardiac arrest procedures, is administered every 3-5 minutes, aiming to increase coronary and cerebral perfusion, The adult cardiac arrest algorithm also provides guidance on managing reversible causes, like the Hs and Ts of ACLS.
Throughout the code, ACLS emphasizes teamwork, frequent reassessment, and optimization of CPR quality. The goal is to provide the highest quality CPR and avoid pauses that can be detrimental. Following the algorithm while tailoring it to each specific cardiac arrest scenario is key.
Recognizing Signs of Spontaneous Circulation
Return of spontaneous circulation(ROSC) is the resumption of sustained cardiac activity due to significant perfusion of the heart. The sign of ROSC includes breathing, coughing, or movement along with the sign of a palpable pulse or measurable blood pressure.
End-tidal CO2 (PETCO2) readings are instrumental in detecting a return of spontaneous circulation (ROSC). A sustained increase in PETCO2, particularly above 25 mm Hg, is an indicator of ROSC. A rise above 40 mm Hg typically confirms ROSC. Traditional methods, monitoring for a pulse and observing blood pressure, remain foundational in detecting spontaneous circulation.
Shock Delivery and Medications
Biphasic defibrillators have become the gold standard in many institutions, including Heart Start CPR. The ability of these devices to adjust their energy output based on impedance is invaluable. When uncertain of the exact energy to use, opting for the maximum available is often the best course of action.
Drug therapy during resuscitation has its own set of challenges and considerations.
Reversible Causes
The H's and T's—the potentially reversible causes of cardiac arrest—serve as a mnemonic checklist that has proven invaluable during the chaos of a code. From Hypovolemia to Thrombosis, each potential cause demands a different intervention, and identifying and addressing the correct one can mean the difference between life and death, following the guidelines of the adult cardiac arrest algorithm. Reversible causes can be:
- Hypovolemia
- Hypoxia
- Hydrogen ion (acidosis)
- Hypo-/Hyperkale
- Tension pneumothorax
- Tamponade, cardiac
- Toxins
- Thrombosis, pulmonary
- Thrombosis, coronary
Final thoughts
The ACLS algorithm, while systematic and structured, requires more than rote memorization—it demands intuition, experience, and the ability to remain calm under pressure. Every cardiac arrest algorithm scenario is unique, but having a solid foundation and understanding of the ACLS cardiac arrest algorithm has been indispensable in my professional journey.
FAQs of ACLS Cardiac Arrest Algorithm
Healthcare providers preparing for their ACLS renewal or attempting it for the first time should memorize the algorithm properly. Below are the common questions frequently asked by students:
What are the steps in ACLS cardiac arrest algorithm?
Recognition, CPR, shock delivery, advanced airway management, and medication are the steps of the ACLS cardiac arrest algorithm. The steps are simple yet must be monitored and addressed according to the algorithm. The steps of the algorithm provide a structured approach for healthcare providers to assess and treat patients.
What is the first drug of choice in a cardiac arrest according ACLS guidelines?
Epinephrine is the primary drug that is provided to a patient suffering from cardiac arrest according to the AHA ACLS protocol. Epinephrine helps to increase heart rate and blood pressure, however, a rescuer should follow specific guidelines for the timing and dosage. Epinephrine acts by binding to alpha-1 receptors, causing smooth muscles in blood vessels to contract, leading to increased blood pressure. It also contracts the pupillary dilator muscles in the eyes and the intestinal sphincter muscles. Additionally, it stimulates beta-1 receptors, increasing heart rate, strengthening heart contractions, and triggering renin release, all of which can be beneficial in managing cardiac arrest and other emergency situations.
What are the 3 shockable rhythms?
Ventricular Tachycardia, Ventricular Fibrillation, and Supraventricular Tachycardia are the 3 shockable rhythms. While following the adult cardiac arrest algorithm guidelines, check pulse for no more than 10 seconds every 2 minutes. On indication of V-Fib and V-Tach shockable rhythm, prepare to shock the patient.
Do you give epinephrine in V-tach?
Epinephrine is commonly used in the treatment of ventricular tachycardia (V-tach) when it is associated with a pulse, which means the heart is still pumping blood. In this case, it is administered as part of AHA advanced cardiac life support (ACLS) protocols to improve cardiac output and blood pressure. However, if V-tach degenerates into ventricular fibrillation (V-fib) or pulseless ventricular tachycardia, defibrillation is usually the primary intervention, and epinephrine may be administered as part of the resuscitation efforts. The use of epinephrine in specific situations depends on the patient's condition and the clinical judgment of healthcare providers.
Do you shock VT with a pulse?
No, you typically do not shock ventricular tachycardia (V-tach) when the patient has a pulse. V-tach with a pulse is a life-threatening arrhythmia, but it means that the heart is still effectively pumping blood. In such cases, the treatment involves addressing the underlying cause of V-tach and administering medications like anti-arrhythmics (e.g., amiodarone) or other interventions to stabilize the heart rhythm and blood pressure. Electrical cardioversion (shock) is reserved for unstable V-tach (where the patient has a pulse but is showing signs of deterioration) or for certain other cardiac arrhythmias.
What is the first medication for pulseless VT?
Amiodarone and epinephrine are commonly used medications for pulseless ventricular tachycardia (VT). Usually, 1mg of epinephrine should be given every 3-5 minutes for a pulseless VT while the medicine can be replaced by vasopressin given 40 units IV once.
Why is asystole not shockable?
Asystole is a condition where the heart completely stops working, and the absence of electrical activity in the heart is shut down. In other words, the heart is not producing any organized electrical impulses, and there is no coordinated contraction of the cardiac muscle. In this state, there is nothing to "shock" or defibrillate because there are no abnormal rhythms or electrical waves to reset. Defibrillation can help to reset the heart's electrical system and potentially restore a normal rhythm only if there is any disorganized electrical activity in the heart such as ventricular fibrillation (V-fib) or pulseless ventricular tachycardia (V-tach).
What does ROSC stands for?
ROSC stands for Return of Spontaneous Circulation. It is not a medical condition but rather a critical event in emergency medicine. ROSC occurs when, during the management of a cardiac arrest or other life-threatening situation, a patient's heart regains the ability to contract and pump blood on its own. It signifies a return of organized, spontaneous cardiac activity and is a positive outcome during resuscitation efforts. After verifying ROSC immediately follow the post-cardiac arrest algorithm in order to optimize the outcomes.
Fast and Convenient
Take ACLS Classes
*Nationally Accepted
ACLS
CERTIFICATION
AHA ACLS course
State-of-the-Art Facilities
Unlimited Exam Retakes
$260
ACLS
ONLINE CERTIFICATION
AHA ACLS Online Course
100% online training
Unlimited Exam Retakes
$280