Pediatric Septic Shock Algorithm

Septic shock remains a leading cause of morbidity and mortality in children worldwide. Rapid recognition and timely management are crucial to improving outcomes. The pediatric septic shock algorithm outlines an evidence-based approach to the initial resuscitation and management of children with septic shock.
The priorities include airway management, establishment of adequate vascular access, administration of fluid and vasopressor boluses, prompt initiation of broad-spectrum antibiotics, and transfer to intensive care. Following the algorithm helps standardize care across different providers and healthcare settings. When implemented effectively, the pediatric septic shock algorithm has been shown to reduce mortality rates to less than 10%.
This article will provide an overview of the key steps in the algorithm, the rationale behind them, and the clinical evidence supporting their use. The intended audience is medical students and clinicians who care for critically ill children at risk of septic shock. A strong understanding of the pediatric septic shock algorithm is essential for providing timely recognition and treatment for this high-risk condition.
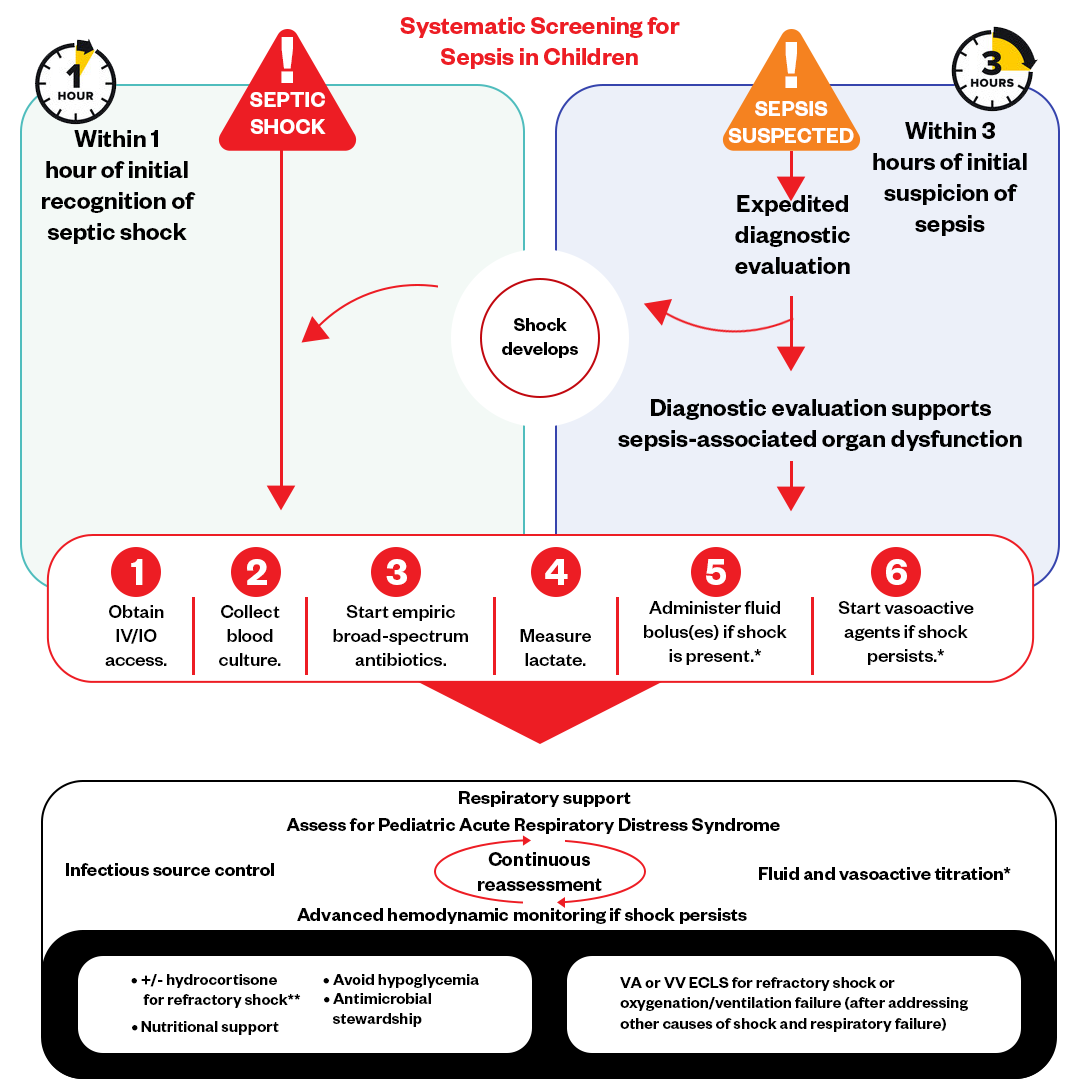
Figure: Pediatric Septic Shock Algorithm
Recognition of the Sepsis
Early recognition of sepsis is critical, as delay in treatment worsens outcomes. Signs and symptoms suggestive of sepsis include:
- Fever or hypothermia
- Tachycardia
- Tachypnea
- Altered mental status
- Flushing, mottling, or cyanosis of skin
- Delayed capillary refill
- Lactic acidosis
- Oliguria
- Hyperglycemia
Diagnostic criteria for sepsis require a suspected infection plus ≥2 age-specific systemic inflammatory response syndrome (SIRS) criteria, including temperature, heart rate, respiratory rate, and white blood cell count abnormalities.
Warm Shock vs. Cold Shock
Warm Shock vs. Cold Shock
Warm shock is the more common presentation of pediatric septic shock. It involves vasodilation, normal or bounding pulses, flashing capillary refill, and warm extremities.
Cold shock involves significant vasoconstriction leading to weak pulses, delayed capillary refill, cool extremities, and low cardiac output. It is more likely with certain pathogens like meningococcus.
Distinguishing warm vs. cold shock guides management. Warm shock benefits more from vasopressor administration, while cold shock requires aggressive fluid resuscitation first to improve cardiac output and perfusion.
Early recognition of sepsis signs, diagnostic evaluation for suspected infection, and distinguishing warm versus cold shock are imperative for the rapid implementation of the pediatric sepsis algorithm. This allows goal-directed therapy tailored to the shock subtype.
Management and Drug Therapy for Septic Shock
When implementing the pediatric septic shock algorithm goals are to improve perfusion and mental status, normalize lactate levels and vital signs, and avoid fluid overload and edema. Rapid fluid resuscitation with isotonic fluids and vasoactive medications aims to restore perfusion and blood pressure to end-organ beds like the brain, heart, and kidneys. This helps improve mental status and avoid long-term neurological deficits.
Normalizing lactate, which is a marker of tissue hypoperfusion, and vital signs indicate the interventions are effectively restoring hemodynamic stability. However, aggressive fluid administration comes with risks of pulmonary edema and fluid overload. Careful monitoring and avoidance of over-resuscitation are important.
Using the Pediatric Septic Shock Algorithm helps strike the right balance between rapid restoration of circulation and avoidance of fluid overload complications. Meeting all the key therapeutic goals is essential for the best possible outcomes in pediatric septic shock.
Septic Shock Interventions
Initial Assessment and Resuscitation:
- Quickly assess airway, breathing, circulation, and mental status. Provide supplemental oxygen and intubation if needed.
- Obtain vascular access - at least two peripheral IVs or central lines.
- Draw labs including blood culture, CBC, electrolytes, lactate, blood gas, and glucose.
- Give 20 mL/kg bolus of isotonic fluid over 5-10 minutes.
- Reassess and repeat boluses up to 60 mL/kg in the first 15 minutes.
- Start vasoactive medications if needed after 40-60 mL/kg fluid. First-line is dopamine or epinephrine.
- Treat hypoglycemia if present.
Further Management
- Continue fluid resuscitation - up to 200 mL/kg in the first hour. Monitor for fluid overload.
- Start broad-spectrum antibiotics within 1 hour. Cover for typical bacteria like Streptococcus pneumoniae, Staphylococcus aureus, Escherichia coli, and Pseudomonas aeruginosa.
- Place arterial and central venous catheters to guide further care.
- Give hydrocortisone if fluid refractory shock persists.
- Transfer to pediatric ICU.
Septic Shock Medications
Careful titration of fluids, vasoactive medications, corticosteroids, and antibiotics, as guided by the pediatric sepsis algorithm, provides the pharmacologic support needed in septic shock.
Here is an overview of some critical medications used in the management of pediatric septic shock:
Fluids:
- Isotonic crystalloids (normal saline, lactated Ringer’s) are the first line for volume resuscitation. The initial bolus is 20 mL/kg in the first 15 min.
- Vasopressors/Inotropes
- Dopamine and epinephrine are the most commonly used vasopressors. Start after 40-60 mL/kg fluid if poor perfusion persists.
- Dobutamine is an inotrope sometimes added for myocardial dysfunction. Strengthens cardiac contractions.
- Norepinephrine can be added if blood pressure remains low despite other vasopressors. Potent peripheral vasoconstrictor.
Corticosteroids:
- Hydrocortisone can help treat fluid-refractory shock. The dose is 1-2 mg/kg/dose every 6 hrs.
- Improves vasopressor responsiveness.
Antibiotics:
Broad-spectrum empiric therapy should be started within 1 hour. Common choices include:
- Ceftriaxone
- Vancomycin
- Piperacillin-tazobactam
- Carbapenems (meropenem, imipenem)
Other:
- Vasopressin may be trialed for refractory shock, which is not responsive to other agents.
- Calcium and bicarbonate replenishment may be needed if hypocalcemia or lactic acidosis occurs.
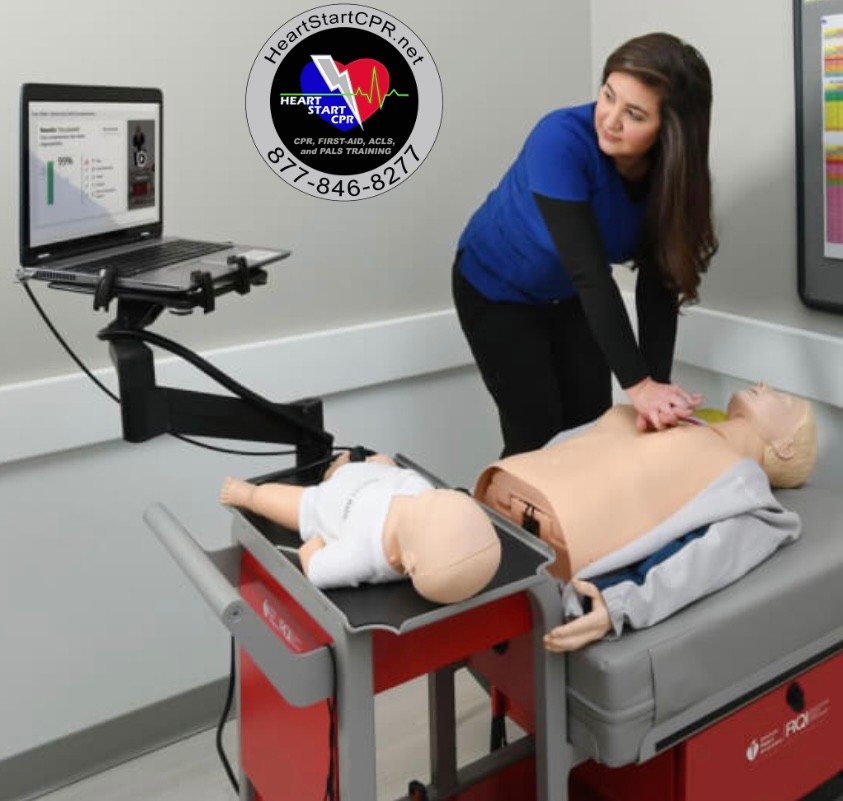
Fast and Convenient
Take PALS Classes
*Nationally Accepted
PALS
CERTIFICATION
AHA PALS course
State-of-the-Art Facilities
Unlimited Exam Retakes
$260
PALS
ONLINE CERTIFICATION
AHA PALS Online Course
100% online training
Unlimited Exam Retakes
$300