PALS Tachycardia Algorithm

Pediatric tachycardia is an abnormally rapid heart rate in children, typically defined as a heart rate exceeding the normal range for a child's age. Common causes include fever, infection, dehydration, underlying heart disease, arrhythmias, medications or stimulants, pain, and anxiety. Normal heart rate varies by age/size.
| Age Group | Normal Heart Rate (BPM) |
|---|---|
| Newborns (0-1 month) | 120-160 |
| Infants (1-12 months) | 100-150 |
| Toddlers (1-2 years) | 90-140 |
| Preschoolers (3-5 years) | 80-120 |
| Children (6-12 years) | 70-110 |
| Adolescents (13-18 years) |
60-100 |
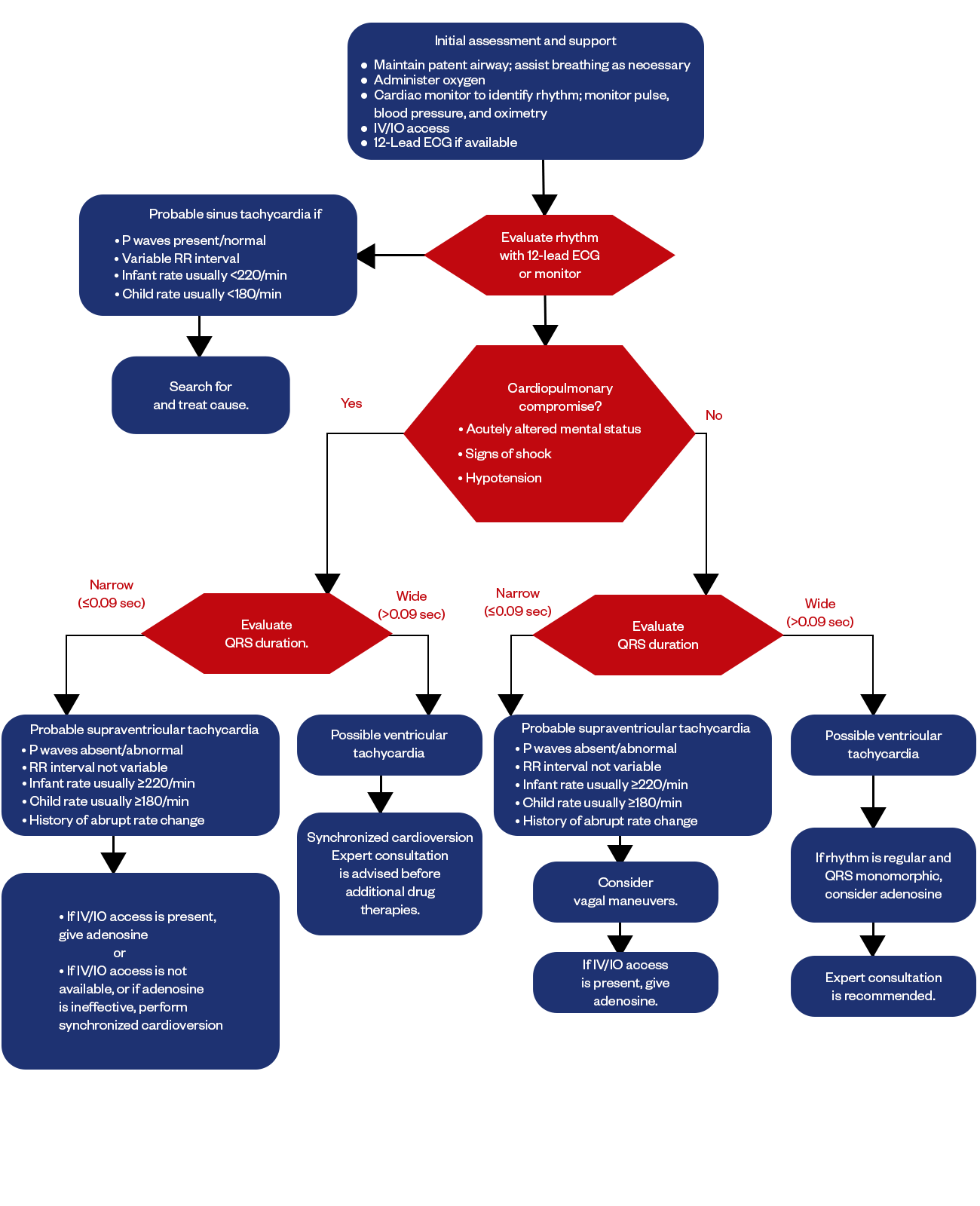
Figure: PALS Tachycardia Algorithm
Tachycardia can be recognized on exam when a child's heart rate is found to be over 180-220 beats per minute in infants and over 140-180 beats per minute in older children. When pediatric tachycardia is identified, the initial assessment should focus on evaluating the stability of the airway, breathing, and circulation, also called ABC, by medical professionals. Attaching a monitor (EKG or ECG) allows determination of the specific rhythm and heart rate.
The algorithmic approach to pediatric tachycardia emphasizes reversibility - first seeking and treating potential underlying triggers like fever or dehydration. Regular, narrow, complex tachycardias may respond to vagal manoeuver or adenosine. Irregular rhythms or those unresponsive to such measures may require antiarrhythmic medications like amiodarone and potentially cardioversion.
The structured algorithm helps organize management, with the goal of identifying causes and unstable rhythms early to guide treatment.
Identify the Type of Tachycardia
Correctly diagnosing the type of tachycardia, finding the underlying cause, and promptly treating both the heart rate and root disorder lead to better outcomes for children affected by abnormally rapid heart rates. Watching for tachycardia provides an important warning sign that further assessment and intervention may be needed.
The types of tachycardia are:
- Supraventricular Tachycardia
- Ventricular Tachycardia
Why Identifying Tachycardia is Important?
- It can be a sign of an underlying medical condition that needs treatment. Some possible causes of pediatric tachycardia include heart defects, low blood pressure, fever, dehydration, anemia, thyroid disorders, electrolyte imbalances, and more.
- Tachycardia increases the risk of cardiovascular complications if left untreated. It can put extra strain on the heart over time and, in some cases, lead to heart failure, especially if there is an underlying heart condition present.
- It can be an early indicator of shock or sepsis, both severe conditions, especially in young children. Catching and treating the tachycardia early on gives a better chance of managing shock or sepsis before they progress too far.
- Some arrhythmias like supraventricular tachycardia (SVT) are more likely to first onset in childhood. Identifying the tachycardia as SVT or another arrhythmia can guide the specific treatment needed.
- It's more important to identify the cause in babies and younger toddlers since they can decompensate quickly. Their smaller size and developing systems make them more vulnerable to cardiovascular insults.
Supraventricular Tachycardia (SVT):
Atrioventricular Nodal Reentrant Tachycardia (AVNRT): This is one of the most common forms of SVT in children. It occurs when there is an abnormal circuit within the heart's atrioventricular (AV) node, leading to rapid heart rates.
Atrioventricular Reentrant Tachycardia (AVRT): AVRT is another form of SVT with an abnormal electrical connection between the atria and ventricles, causing a loop that leads to rapid heartbeats.
Atrial Tachycardia: This type of tachycardia originates in the atria, causing a fast heart rate.
Ventricular Tachycardia (VT):
Ventricular tachycardia is associated with structural heart abnormalities or other underlying heart conditions. Ventricular tachycardia in children is less common than SVT. It involves a rapid heart rate originating in the ventricles, the heart's lower chambers.
Emergency Diagnosis and Management of Pediatric Tachycardia
Initial Assessment and Support
The first step when a child presents with tachycardia is to stabilize them by maintaining an open airway, assisting breathing as needed, administering oxygen, attaching cardiac monitoring, and establishing IV or IO access for giving medications. A 12-lead ECG should also be obtained if available to accurately diagnose the rhythm. Vital signs, including pulse rate, blood pressure, and pulse oximetry, should be continuously monitored.
Evaluating the Rhythm
The next step is determining if the rhythm indicates sinus tachycardia or another concerning rhythm, like ventricular tachycardia, that is compromising cardiopulmonary status.
Sinus tachycardia will still show organized P waves with normal morphology and a variable R-R interval. Rates in infants are typically below 220 bpm and below 180 bpm in older children. If this pattern is seen, possible causes like fever, dehydration, and medications must be searched for and treated.
Concerning signs include very high heart rates, absent/abnormal P waves, and a non-variable R-R interval history of an abrupt rate change. This indicates possible SVT, which requires immediate treatment with adenosine or synchronized cardioversion if the patient is unstable.
A wide QRS complex (>0.09 sec) indicates probable ventricular tachycardia, which also requires immediate cardioversion and expert consultation regarding anti-arrhythmic medications.
Hemodynamically Stable Patients
If the patient has a narrow complex rhythm but is hemodynamically stable, vagal maneuvers can be attempted first to slow the rate down without medications. However, adenosine should be prepared if this is not successful. Regular, monomorphic, wide, complex tachycardia can also respond to a trial of adenosine after expert consultation.
Key Points:
- Identify rhythm, P waves, and QRS duration to diagnose the type of tachycardia.
- Search and treat the underlying cause of sinus tachycardia.
- Cardiovert unstable SVT and VT
Try vagal maneuvers first in stable SVT. - Adenosine and antiarrhythmics may be used for refractory cases.
- Expert consultation is advised for ventricular rhythms or unstable patients.
Drug Therapy
Adenosine
- First-line medication for stable SVT
- Works by temporarily blocking the AV node to interrupt the tachycardia circuit
- Rapid onset is useful in an emergency setting.
- Given as rapid IV push at an initial dose of 0.1 mg/kg (maximum 6 mg)
- The second dose can be given at 0.2 mg/kg if needed (maximum 12 mg)
- Side effects include chest pain, flushing, and dyspnea.
Procainamide
- Anti-arrhythmic used second-line for SVT or VT
- Loading dose 10-15 mg/kg over 30-60 min, then maintenance infusion
- Monitor ECG blood pressure, avoid hypotension
- Side effects: nausea, QT prolongation, lupus-like reaction with prolonged use
- Amiodarone
- Excellent pediatric anti-arrhythmic, though not FDA-approved
- Broad spectrum - treats SVT, VT, Afib/flutter
IV loading 5 mg/kg over 60 min followed by infusion - Hypotension is a common side effect requiring pressure
Esmolol
- Short-acting beta blocker proper if adenosine fails in SVT
- Loading dose 500 mcg/kg/min followed by 50-300 mcg/kg/min infusion
- Side effects include bradycardia, hypotension, bronchospasm
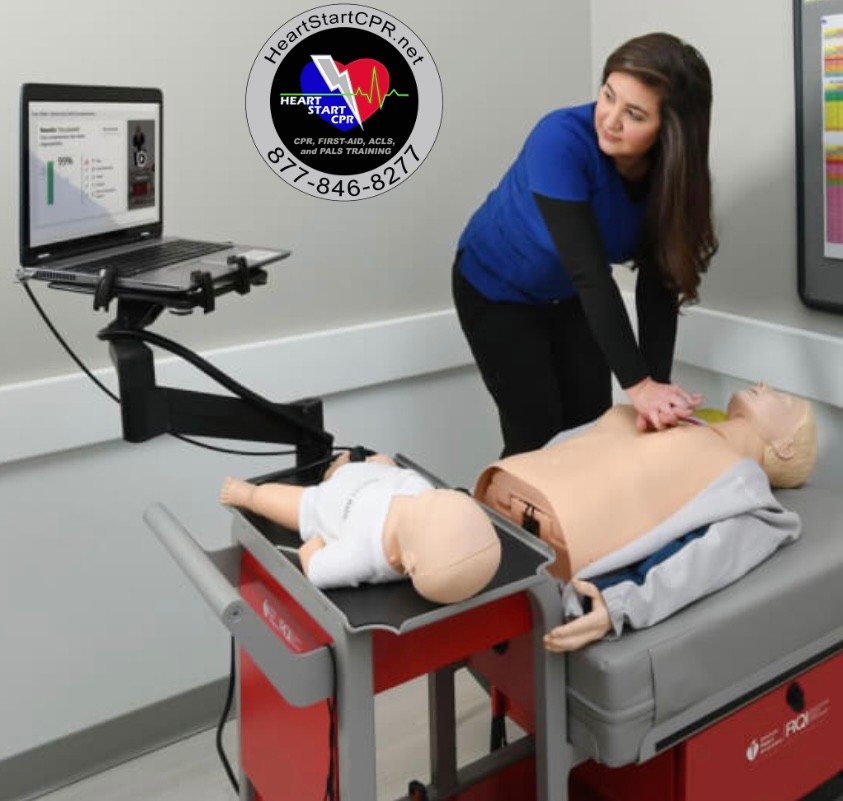
Fast and Convenient
Take PALS Classes
*Nationally Accepted
PALS
CERTIFICATION
AHA PALS course
State-of-the-Art Facilities
Unlimited Exam Retakes
$260
PALS
ONLINE CERTIFICATION
AHA PALS Online Course
100% online training
Unlimited Exam Retakes
$300