Pediatric Cardiac Arrest Algorithm

The pediatric cardiac arrest algorithm provides step-by-step instructions for assessing and treating a child or infant experiencing cardiac arrest in or outside the hospital setting. The algorithm is intended to assess children (<12 years) with cardiac arrest in any setting (in-hospital/outside the hospital).
The algorithm is designed to guide healthcare providers through the critical actions needed to attempt resuscitation and achieve a return of spontaneous circulation (ROSC). The key components of the algorithm include immediate recognition and activation of the emergency response system, high-quality CPR, defibrillation when appropriate, and post-cardiac arrest care.
The pediatric cardiac arrest algorithm below is updated and based on the “7th annual summary publications of the International Liaison Committee on Resuscitation (ILCOR) International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations (CoSTR)” published between 2022 and 2023.
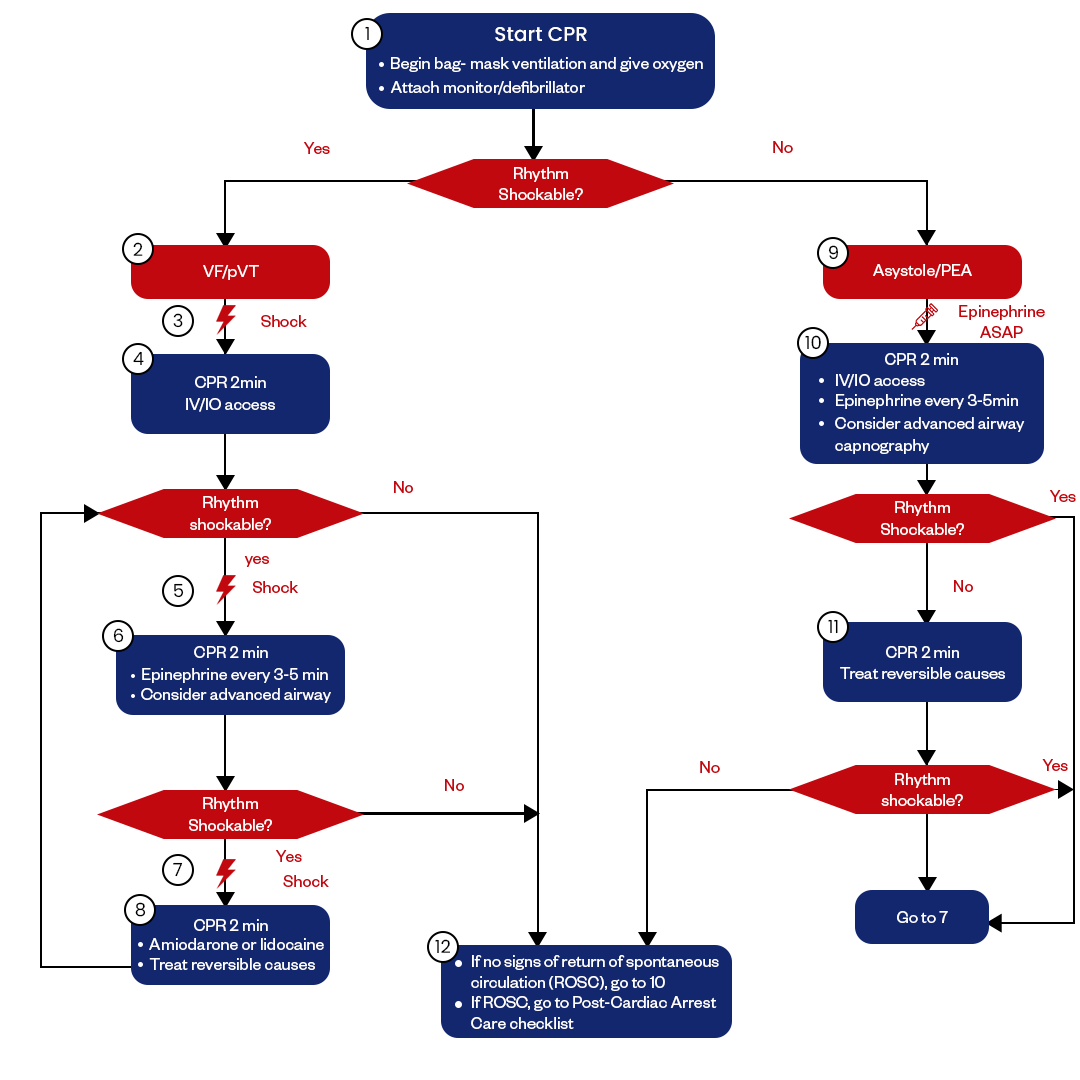
Figure: PALS Cardiac Arrest Algorithm
Basic Life Support
PALS BLS algorithm prepares single-rescuer and multiple-rescuer teams to deliver high-quality CPR and initiate initial assessment for infants and children.
Before the arrival of advanced life support, the pediatric cardiac arrest algorithm begins with an assessment for responsiveness. If the child is unresponsive with no breathing or only gasping, high-quality child CPR should be initiated immediately. Provide rescue breaths followed by cycles of 30 compressions and 2 breaths.
A compression-to-ventilation ratio of 15:2 can be used for 2 rescuers. Adequate depth and rate of compressions are critical - at least 1/3 AP depth for infants and 1/3 to 1/2 AP depth for children at a rate of 100-120 compressions per minute.
Advanced Life Support
Once additional emergency responders arrive, the algorithm follows advanced cardiac life support guidelines. Establish vascular access and administer epinephrine every 3-5 minutes. Replace epinephrine with vasopressin for refractory ventricular fibrillation or pulseless ventricular tachycardia.
If a shockable rhythm is identified, provide immediate defibrillation. A dose of 2-4 J/kg is recommended for the first defibrillation attempt, with subsequent doses of 4 J/kg. Amiodarone and lidocaine can be given for refractory ventricular fibrillation/pulseless ventricular tachycardia. Correct reversible causes throughout resuscitation efforts.
Signs of Pediatric Cardiac Arrest
The most obvious and immediate sign that a pediatric patient has experienced cardiac arrest is a sudden loss of consciousness with the absence of normal breathing. Gasping resuscitation may occur initially but will stop. There will be no palpable pulses, no signs of circulation or spontaneous movement, and the child will be unresponsive to stimuli. Skin signs like pallor, mottling, or cyanosis often become apparent quickly as circulation ceases.
Using assessment aids like stethoscopes, providers may hear abnormal heart sounds like PEA or observe heart rhythms on monitors incompatible with adequate blood circulation. Vital signs are always absent when a true cardiac arrest has occurred. Once identified, the pediatric cardiac life support algorithm should be immediately implemented while determining and reversing the underlying cause of arrest. Ongoing assessment for signs of return of spontaneous circulation is critical during the resuscitation efforts.
Here are the key signs and symptoms of pediatric cardiac arrest:
- Unresponsiveness
- Lack of normal breathing or only gasping respirations
- No signs of circulation, such as coughing, movement, or normal breathing
- Pallor or cyanosis of the skin
- Absent pulse
- Dilated pupils
- Loss of tone, so the child feels limp or floppy
- Brassy heart sounds or silence on auscultation
- Cardiac rhythm showing asystole, pulseless electrical activity, ventricular fibrillation, or ventricular tachycardia
Treatment of Pediatric Cardiac Arrest
Cardiac arrest in children requires prompt and effective treatment to give the patient the best chance of survival and positive neurological outcomes. The approach to pediatric cardiac arrest focuses on high-quality chest compressions, early defibrillation when indicated, optimal airway management and ventilation, and appropriate medications.
Chest Compression
Chest compressions are a critical component of pediatric resuscitation, with guidelines emphasizing compressions at a rate of 100-120 per minute to a depth of at least one-third the anterior-posterior diameter of the chest. Effective compressions generate blood flow and perfusion to vital organs. The table below clearly shows the AHA guidelines regarding chest compression and CPR:
| Compression Rate | 100-120 compressions per minute |
|---|---|
| Depth | Adolescents: 5–6 cm Children: approximately 5 cm (≥one-third anterior-posterior chest depth) Infants: approximately 4 cm (≥one-third anterior-posterior chest depth) |
| Fraction | 80% of the total cardiac arrest time |
| Chest Recoil | Allow complete recoil of chest compressions |
| Ventilations | Advanced airway: 10 breaths/min No advanced airway (adolescents): 30:2 compression to ventilation ratio No advanced airway (children and infants): 15:2 compression to ventilation-ratio |
Optimal Pediatric Airway Management
Basic airway maneuvers and bag-mask ventilation remain the recommended first-line strategies for oxygenation and ventilation during pediatric cardiac arrest. An observational cohort study, using the All-Japan Utstein Registry between 2014 and 2016 led by Mashashi Okubo and teams named “Prehospital advanced airway management for pediatric patients with out-of-hospital cardiac arrest: A nationwide cohort study” in Japan found that infants and children with non-shockable rhythms, opening the airway with basic maneuvers led to improved survival compared to the use of an advanced airway. Bag-mask ventilation is effective at oxygenating and ventilating pediatric patients. When performed correctly, bag-mask ventilation can achieve adequate oxygen saturation in 92% of pediatric cardiac arrest patients. Rescuers should focus on providing effective ventilations with room air or supplemental oxygen using a bag-mask device before considering advanced airways.
If bag-mask ventilation does not provide adequate oxygenation and ventilation, insertion of an advanced airway becomes necessary. Endotracheal intubation has been considered the gold standard, as it best protects the airway, provides the most reliable ventilation, and enables capnography monitoring. However, intubation does require interrupting chest compressions. Alternatives like the Laryngeal Mask Airway (LMA) can also facilitate oxygenation and ventilation. The study led by Mashashi Okubo team (DOI: 10.1016/j.resuscitation.2019.09.007) in Japan found no difference in 30-day survival between endotracheal intubation and LMA insertion. Conclusion: The choice of airway can be based on provider experience and patient factors.
Importantly, research has shown that advanced airway placement negatively impacts survival if interrupting compressions for >3 minutes, as documented in a journal “Association Between Tracheal Intubation During Pediatric In-Hospital Cardiac Arrest and Survival” (DOI: 10.1001/jama.2016.14486). To minimize this impact, airway placement should occur rapidly during planned compression pauses, with a goal of <10 seconds per pause. This organized approach also requires at least 2 trained and skilled providers to efficiently coordinate airway management around continuous high-quality chest compressions, which neurologically vulnerable pediatric patients rely heavily on.
Defibrillation
Promptly delivered appropriate energy level defibrillation, integrated around uninterrupted compressions, is crucial for pediatric patients in ventricular fibrillation or pulseless ventricular tachycardia to try restoring a perfusing rhythm.
The two rhythms for which defibrillation is indicated in pediatric patients are ventricular fibrillation and pulseless ventricular tachycardia. Defibrillation works by depolarizing the myocardium to help restore organized electrical activity that can generate perfusing rhythms.
Multiple studies have shown better outcomes when shocks are delivered promptly for pediatric shockable rhythms. Quicker time to first shock is associated with improved ROSC and survival rates. As such, rapidly retrieving and preparing defibrillator equipment is a priority when shockable rhythms are identified.
The recommended initial energy dose for defibrillation on a child experiencing cardiac arrest is 2 J/kg, followed by second and subsequent doses of 4 J/kg if the initial shock is unsuccessful. Higher energy doses have not proven more efficacious in pediatric patients. Biphasic waveforms are preferred over monophasic forms for better efficacy and outcomes.
To avoid interruptions in chest compressions, the defibrillation strategy should be coordinated around rhythm checks and pulse checks with planned pauses. Compressions should be resumed immediately after shock delivery and not paused until rhythm reassessment.
Here is a step-by-step guide for defibrillation in pediatric cardiac arrest:
Defibrillation Pad Size, Type, and Placement:
- Use pediatric-sized pads if available. Standard adult pads are acceptable if pediatric pads are unavailable.
- For children < 10 kg, use infant/child pads in the anterior-posterior (front-back) position.
- For children > 10 kg, place pads in the standard anterior-lateral position.
Energy Doses:
- First shock: 2 J/kg
- Second and subsequent shocks: 4 J/kg
- Biphasic waveform preferred over monophasic waveform
Shock Sequence:
- Single shocks are recommended over stacked shocks
- Resume chest compressions immediately after each shock once the rhythm is reassessed
- Coordinate single shocks with pulse and rhythm checks during planned compression pauses every 2 minutes
- Avoid interruptions in compressions for shock delivery and rhythm analysis > 10 seconds
Medication
The medication related to pediatric cardiac arrest are Epinephrine, Vasopressin, and Antiarrhythmics. Epinephrine is the first-line vasopressor, amiodarone is used for shock-refractory ventricular arrhythmias, and calcium/bicarb are adjunctive therapies for specific situations in pediatric cardiac arrest. The priority is prompt, high-quality chest compressions along with defibrillation when indicated. Here is an overview of the key medications used in pediatric cardiac arrest:
Epinephrine:
- Epinephrine is the first-line vasopressor.
- The potent alpha and beta-adrenergic agent that stimulates cardiac contraction, vascular tone
- Recommended every 3-5 minutes in pediatric cardiac arrest
- Causes vasoconstriction and increases coronary perfusion pressure to facilitate the return of spontaneous circulation
- The drug is typically given IV/IO route 0.01 mg/kg (0.1 mL/kg of 0.1 mg/mL concentration)
Vasopressin:
- It can be used as an alternative pressor to epinephrine
- Works on V1 receptors to cause vasoconstriction
- Dose 0.4-1 units/kg IV/IO, up to 40 units maximum
Antiarrhythmics:
- Amiodarone - for refractory ventricular fibrillation/tachycardia
- Works by blocking potassium channels to prolong action potential
- 5 mg/kg IV/IO bolus during cardiac arrest
Reversible Causes
Rapid evaluation for reversible factors should occur immediately, as prompt identification and treatment are associated with markedly improved survival rates. Continually reassessing for possible contributing and evolving factors during the pediatric arrest can also optimize management and outcome.
It is vital to identify and rapidly treat any reversible causes of pediatric cardiac arrest. First, determining the underlying etiology can dictate specific interventions during the resuscitation, such as glucose for hypoglycemia. Second, addressing reversible factors maximizes the patient's chance for a positive outcome.
The American Heart Association emphasizes diagnosing and treating reversible causes as a critical component of pediatric cardiac arrest care. Causes like hypoxia, hypovolemia, acidosis, and hypoglycemia are most common. Identifying less frequent causes like tension pneumothorax or toxin exposure can also enable targeted treatment during the “4 Hs and 4 Ts” assessment.
The 4Hs and Ts are:
- Hypovolemia
- Hypoxia
- Hydrogen ion (acidosis)
- Hypoglycemia
- Hypo-/hyperkalemia
- Hypothermia
- Tension pneumothorax
- Tamponade, cardiac
- Toxins
- Thrombosis, pulmonary
- Thrombosis, coronary
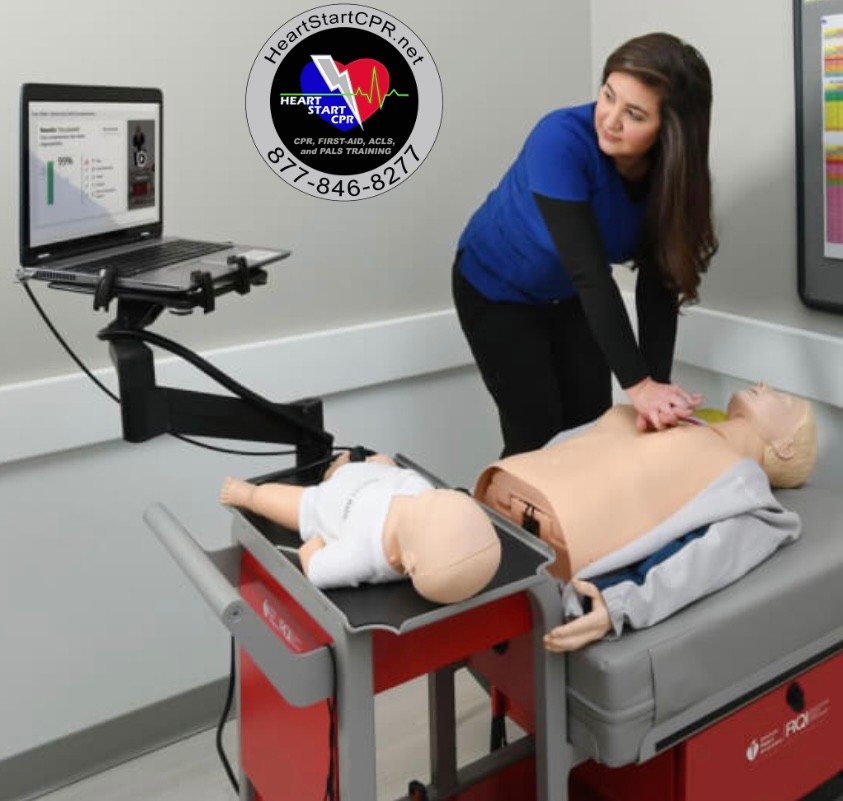
Fast and Convenient
Take PALS Classes
*Nationally Accepted
PALS
CERTIFICATION
AHA PALS course
State-of-the-Art Facilities
Unlimited Exam Retakes
$260
PALS
ONLINE CERTIFICATION
AHA PALS Online Course
100% online training
Unlimited Exam Retakes
$300
Pediatric Cardiac Arrest Algorithm FAQs
What is the first step in the pediatric cardiac arrest algorithm?
The initial assessment for responsiveness guides the immediate activation of emergency resources and the decision of whether cardiac arrest treatment is indicated based on signs of life. Checking responsiveness kicks off the subsequent steps of the pediatric cardiac arrest algorithm flow to either begin life-saving interventions or pursue condition-specific treatments for non-arrest scenarios.
How do you check a child's pulse during cardiac arrest?
In a child, palpate a carotid or femoral pulse. Test no more than 10 seconds to assess the child victim, delayed in CPR delivery can affect the child’s health negatively. The carotid pulse can be found on the one side of the neck near the windpipe, gently press to feel the pulse. Similarly, to find the femoral pulse in a child, place your fingertips over the anterior hip crease, you can feel the pulsation.
What is the most common rhythm in pediatric cardiac arrest?
Asystole and Bradycardia are the most common rhythms documented in in-hospital settings. Whereas 10-14% of patients are reported with Ventricular fibrillation or pulseless ventricular tachycardia.
What if a child has no pulse after 2 minutes?
If a child has no pulse after 2 minutes, activate the emergency response system (if not already initiated), then immediately commence CPR. Continue CPR until prompted by an AED for a rhythm check, ensuring continuous lifesaving measures.

Owner Jeff Haughy has been providing high-quality care in the EMS industry since 1995 and started his Fire Service career with the Alameda Fire Department in 1991 as a Fire Explorer.