PALS Bradycardia Algorithm

Pediatric Bradycardia is a condition of having a low heart rate below the normal range in a child. The normal heart rate in a child varies according to the age, for example, a newborn baby’s heart beats at the rate of 80-205 times per minute, more information is given in the table below. Bradycardia needs to be identified, including its cause and types, and a diagnosis needs to be provided accordingly. Once the symptomatic bradycardia is recognized in a child, the systematic approach algorithm is used to direct the care.
The below table shows the normal heart rate (BPM) of a child according to their age:
| Age Group | Normal Heart Rate (BPM) |
|---|---|
| Newborns (0-1 month) | 120-160 |
| Infants (1-12 months) | 100-150 |
| Toddlers (1-2 years) | 90-140 |
| Preschoolers (3-5 years) | 80-120 |
| Children (6-12 years) | 70-110 |
| Adolescents (13-18 years) |
60-100 |
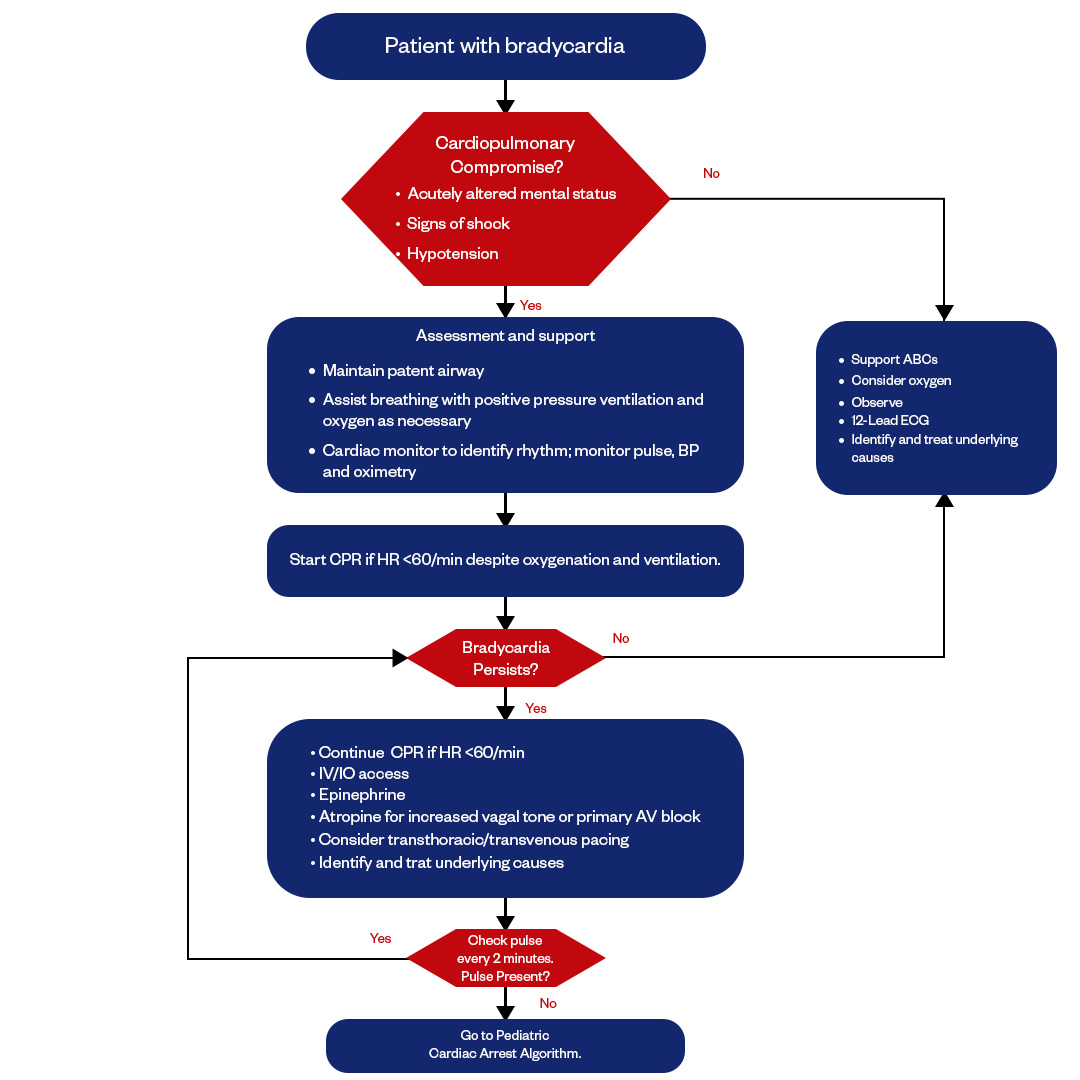
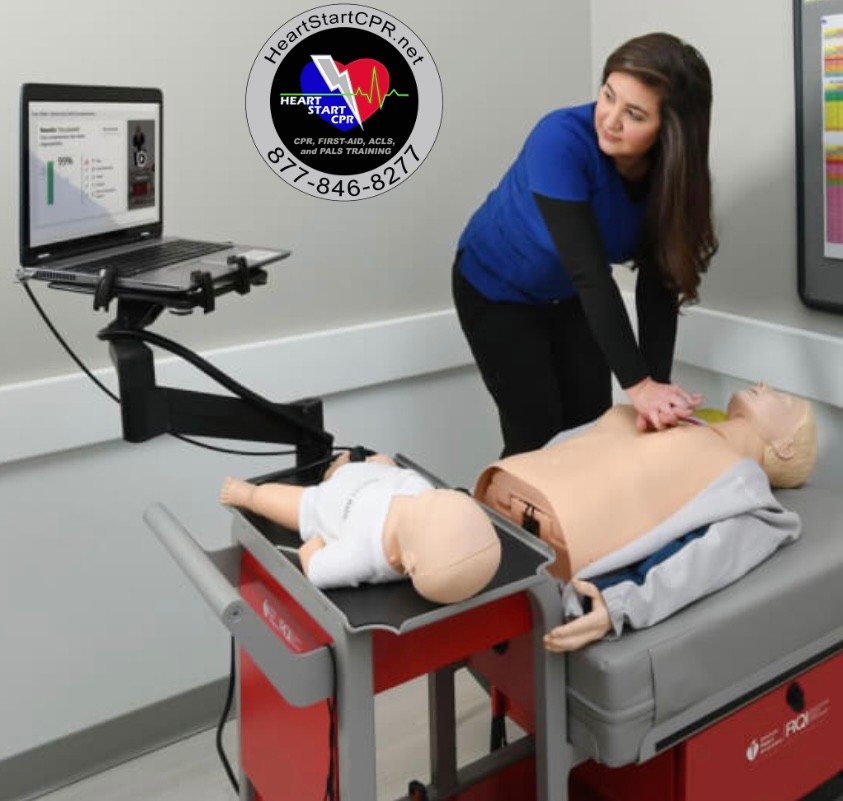
Figure: Pediatric Bradycardia Algorithm
The pediatric advanced life support (PALS) bradycardia algorithm provides a systematic approach for assessing and managing children presenting with symptomatic bradycardia. The algorithm helps healthcare providers rapidly diagnose the cause, stabilize the patient, and provide appropriate interventions based on the clinical presentation.
Key aspects of the PALS algorithm include administering oxygen, monitoring vital signs, assessing perfusion, and preparing for CPR if the patient's condition deteriorates. Following the PALS bradycardia algorithm facilitates rapid decision-making and timely intervention for pediatric patients.
Identify the Bradycardia
To identify bradycardia in a pediatric population, assess the child’s heart rate and compare it to the normal range of their age group. If the heart rate is below the threshold, they have bradycardia. The next step is to determine if the bradycardia is symptomatic or asymptomatic. Signs and symptoms that may be seen with symptomatic pediatric bradycardia include:
- Decreased heart rate
- Hypotension
- Altered mental status
- Pallor
- Cyanosis
- Respiratory distress
- Decreased peripheral perfusion
- Reduced urine output
A systematic approach should then be taken to identify the potential causes of bradycardia based on the clinical presentation. This includes obtaining a history and physical examination, reviewing medications, analyzing ECG morphology, and measuring electrolyte levels. Identifying the cause will then direct appropriate acute management and treatment interventions. The PALS bradycardia algorithm provides a standardized framework for this assessment and diagnosis process, which is discussed in the “Diagnosis and Management” section below. Before that, let’s look at the primary and secondary bradycardia in pediatrics.
Primary Bradycardia
Primary bradycardia is the occurrence of fetal heart rate (FHR) due to heart-related abnormalities. Some of the main causes of primary bradycardia in a child are:
Congenital heart block:
This occurs when there is a delay or interruption in the electrical signal from the heart's upper chambers (atria) to the lower chambers (ventricles). This can result from genetic factors, infections during pregnancy, immune disorders in the fetus, etc.
Sick sinus syndrome:
This refers to improper sinus node function, resulting in an insufficient heart rate. It can be caused by abnormal development or damage to the sinus node.
Myocarditis:
Inflammation/infection of the heart muscle (myocardium) can slow electrical conduction and reduce heart rate. Viruses are a common culprit.
Cardiomyopathy:
The disease of the actual heart muscle can disrupt electrical signals and impair pumping ability. Dilated and hypertrophic cardiomyopathy are forms that can manifest as bradycardia.
Metabolic abnormalities:
Electrolyte disturbances like high blood potassium and low calcium or magnesium levels can slow electrical signaling. Hypothyroidism and low body temperature can also contribute.
Secondary Bradycardia
Secondary bradycardia is the abnormal functioning of the heart caused by non-cardiac problems. Some of the main causes of secondary bradycardia are:
Hypoxemia:
Lack of oxygen reaching the heart can trigger a reflex bradycardia. This is often seen in respiratory distress from pneumonia, bronchiolitis, and asthma exacerbations.
Hypothermia
Low core body temperature reduces metabolic processes and slows pacemaking functions in the heart's electrical conduction system.
Electrolyte imbalances
Abnormally high or low blood sodium, potassium, calcium, or magnesium levels disrupt electrical signaling. Common in dehydration/overhydration.
Toxins/substances
Overdose of medications like beta-blockers, calcium channel blockers, and clonidine, or ingestion of alcohol, illicit drugs, or poisoning can cause bradycardia.
Increased vagal tone
Stimulation of the vagus cranial nerve slows electrical conduction to the heart. Seen with seizures, vomiting, straining, or rectal/eye/ear exams.
Management and Drug Therapy of Bradycardia in Pediatric
Management of bradycardia in pediatric patients involves identifying and treating the underlying cause, as well as providing supportive care if necessary. In some cases, drug therapy may be required.
Management
Identifying and Treating Underlying Causes:
- Hypoxia: Ensure adequate oxygenation.
- Electrolyte Imbalances: Correct any electrolyte abnormalities, such as low potassium or magnesium levels.
- Infection: Treat any infections that may be causing bradycardia.
- Cardiac Structural Abnormalities: Address structural issues if present.
Supportive Care:
- Airway Management: Ensure a patent airway.
- Ventilation Support: Provide mechanical ventilation if necessary.
- Intravenous Fluids: Maintain adequate hydration.
Drug Therapy
- Atropine: An anticholinergic drug that increases heart rate by blocking vagal tone. The initial dose is 0.02 mg/kg (minimum dose 0.1 mg), which may be repeated every 3-5 minutes to a maximum dose of 0.04 mg/kg or 1 mg total.
- Epinephrine: Sympathomimetic, increases heart rate by stimulating beta-1 receptors. IV dose 0.01 mg/kg (1:10,000 solution), repeat every 3-5 minutes.
- Dopamine: Inotrope and chronotrope, dosage 2-20 mcg/kg/min titrated to effect. Often used if epinephrine is ineffective.
Reversible Causes of Symptomatic Bradycardia
- Hypoxemia - Provide supplemental oxygen
- Hypothermia - Rewarm the child, warm IV fluids
- Increased intracranial pressure - Elevate the head of the bed, hyperventilate, consider mannitol/furosemide
- Electrolyte disturbances (hyperkalemia, hypokalemia, hypocalcemia, acidosis) - Correct underlying disorder
- Drug effects - Consider antidotes like atropine for beta blockers or calcium for calcium channel blockers
Fast and Convenient
Take PALS Classes
*Nationally Accepted
PALS
CERTIFICATION
AHA PALS course
State-of-the-Art Facilities
Unlimited Exam Retakes
$260
PALS
ONLINE CERTIFICATION
AHA PALS Online Course
100% online training
Unlimited Exam Retakes
$300