ACLS In-Hospital Cardiac Arrest in Pregnancy Algorithm

The cardiac arrest in pregnancy is rare, occurring in only 1 in 30,000 pregnancies but carries a significantly higher mortality rate compared to the general population due to the physiological changes in a woman's body and the need to consider the life of both the mother and fetus. The resuscitation techniques for pregnant women are similar to those for other adults, but there are special considerations due to the dual-patient scenario. Thankfully, the ACLS In-Hospital Cardiac Arrest in Pregnancy Algorithm provides a structured, evidence-based approach to managing this critical emergency situation.
By following standard ACLS protocols and algorithms, healthcare providers can ensure they are delivering the highest standard of care, improving outcomes in such emergencies where every second counts and informed actions can make all the difference.
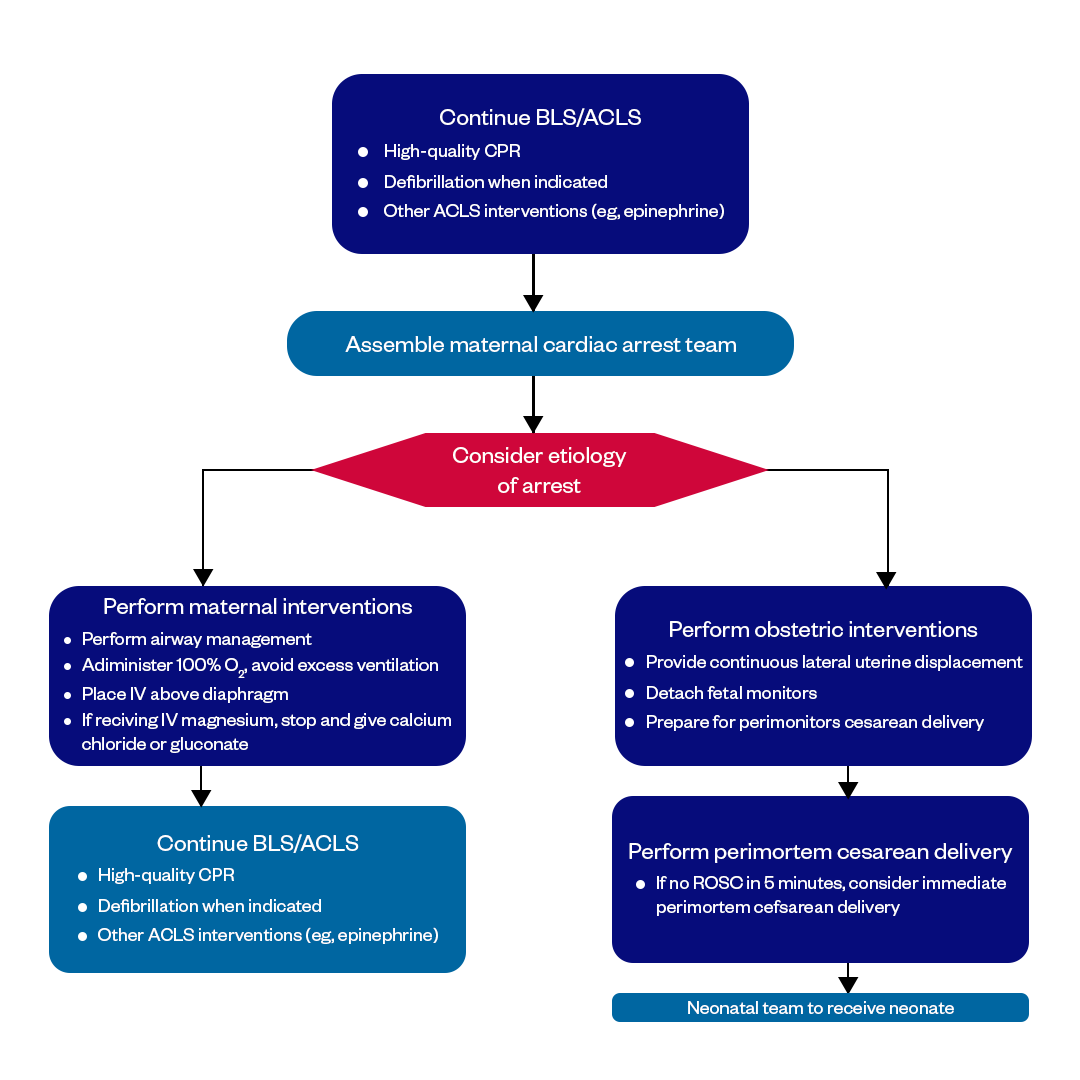
Figure: ACLS In-Hospital Cardiac Arrest in Pregnancy Algorithm
ACLS Protocol and Unique Features for Pregnant Patients
Advanced cardiac life support (ACLS) provides a standardized approach to treating cardiac arrest and resuscitation. The general ACLS algorithm remains the same for pregnant patients with some modifications:
- Prioritize High-Quality Chest Compressions: In pregnant women, high-quality uninterrupted chest compressions are most important to support both mother and fetus by maintaining cardiac output and uteroplacental blood flow. Compressions should be given at a rate of 100-120/minute with full recoil between compressions.
- Early Assessment of Fetal Condition: Assess fetal heart tones as soon as possible after the arrest, usually within 5 minutes of return of spontaneous circulation (ROSC) in mother. Absent fetal heart tones indicate the need for emergency cesarean delivery.
- Modified Positioning: Tilt the mother to her left side if possible instead of supine to relieve pressure from the enlarged uterus on the major blood vessels. This helps improve cardiac preload and uterine blood flow during CPR.
- Consider Early Intubation: Intubation and ventilation may need to be prioritized earlier than the standard 2 minutes if oxygen saturations are low and compromising the fetus. Use a bougie or video laryngoscope for a more guided intubation attempt.
- Optimize Preload: Strategies like left uterine displacement, fluid boluses and vasopressors should be used early to maximize preload and cardiac output aimed at supporting both the mother and fetus.
- Assess Need for Perimortem Cesarean Delivery: Have a low threshold for emergency cesarean delivery if ROSC is not achieved after about 5 minutes of high-quality CPR and defibrillation attempts if indicated. This improves outcomes for the fetus significantly.
The rest of the ACLS algorithm, such as airway management, IV access, cardiac rhythm monitoring, defibrillation, and medication administration, is similar. The main goals are high-quality chest compressions and early consideration of factors unique to pregnancy, like positioning, preload optimization, and fetal assessment/delivery.
Follow the ACLS Algorithm for Pregnant Patients in Cardiac Arrest
Here are the step-by-step recommendations for managing an in-hospital cardiac arrest in pregnancy as per ACLS protocol:
1. Ensure Scene Safety
Ensure provider safety from electrical/chemical hazards before approaching the patient. Organize needed resuscitation equipment and team members.
2. Check Responsiveness
Check for responsiveness by lightly tapping shoulder and shouting "Are you OK?".
3. Activate Emergency Response
Call out "Cardiac arrest!" and send someone to activate emergency response team and 'code blue'.
4. Start Chest Compressions
Begin uninterrupted chest compressions at a rate of 100-120/min with full recoil between compressions. Consider shifting to left lateral tilt as soon as feasible.
5. Attach Cardiac Monitor
Attach cardiac monitor to identify rhythm and look for shockable rhythm like VF/VT. Consider early intubation for ventilation if saturations low.
6. Check Rhythm
Check monitor for shockable (VF/VT) or non-shockable (asystole/PEA) rhythm after 2 minutes of high-quality chest compressions.
7. Defibrillate as Appropriate
For VF/VT, give 1 shock at maximum output and immediately resume compressions for 2 minutes before rechecking rhythm.
8. Continue Chest Compressions
Keep continuous compressions without interruptions except to deliver shocks if indicated. Attempt to minimize pauses to <5 secs.
9. Establish IV Access
Establish IV access preferably above diaphragm as soon as possible without interrupting compressions.
10. Administer Epinephrine
Give Epinephrine 1 mg IV/IO every 3-5 minutes for all non-shockable rhythms (asystole/PEA).
11. Consider Other Drugs/Interventions
Treat reversible causes - H's and T's. Consider vasopressors, fluid boluses, amiodarone as per standard ACLS protocols.
12. Fetal Assessment
Check fetal heart tones as soon as feasible after ROSC, ideally within 5 minutes. Plan for emergency delivery if absent.
13. Assess Need for PMC
If ROSC not achieved after 5 minutes of high-quality CPR, defibrillation attempts if shockable rhythm exists and reversible causes addressed - proceed with perimortem cesarean delivery.
14. Post-Resuscitation Care
If ROSC achieved, focus on hemodynamic/ventilator support, correction of acidosis, cooling, seizures prophylaxis, targeted temperature management.
Final Thoughts
The ACLS algorithm for cardiac arrest in pregnancy aims to resuscitate the mother while actively maintaining oxygenated blood flow to the fetus. A structured, multidisciplinary approach involving obstetric, cardiac, neonatal teams offers the best chance for a positive maternal and fetal outcome in this life-threatening maternal emergency scenario. Close antepartum monitoring and timely resuscitation according to protocol guidelines is critical.
FAQs on ACLS in Pregnancy Cardiac Arrest
What causes cardiac arrest during pregnancy?
- Pre-existing heart conditions like cardiomyopathy
- Pregnancy-induced conditions like preeclampsia, amniotic fluid embolism
- Pulmonary embolism
- Bleeding
- Trauma
- Other medical emergencies
Is defibrillation safe for the fetus?
Yes, defibrillation can be safely administered in a pregnant woman as the high-frequency current does not pass deeply into tissue. No adverse neonatal effects have been demonstrated at standard biphasic energy levels used in cardiopulmonary resuscitation. Rapid defibrillation remains a cornerstone of maternal resuscitation.
Can CPR protocols be safely altered for pregnant patients?
Yes, some key modifications are made to standard CPR protocols when conducting resuscitation efforts on pregnant women. These changes aim to optimize perfusion and oxygen delivery to both the mother and fetus.
Does early delivery after ROSC improve outcomes?
Yes, early delivery within around 30 minutes post ROSC is recommended to optimize both maternal and fetal prognosis. This reduces ischemic placental damage and risk of recurrence of the primary process that led to arrest. The baby also receives prompt resuscitative care.
Fast and Convenient
Take ACLS Classes
*Nationally Accepted
ACLS
CERTIFICATION
AHA ACLS course
State-of-the-Art Facilities
Unlimited Exam Retakes
$260
ACLS
ONLINE CERTIFICATION
AHA ACLS Online Course
100% online training
Unlimited Exam Retakes
$280